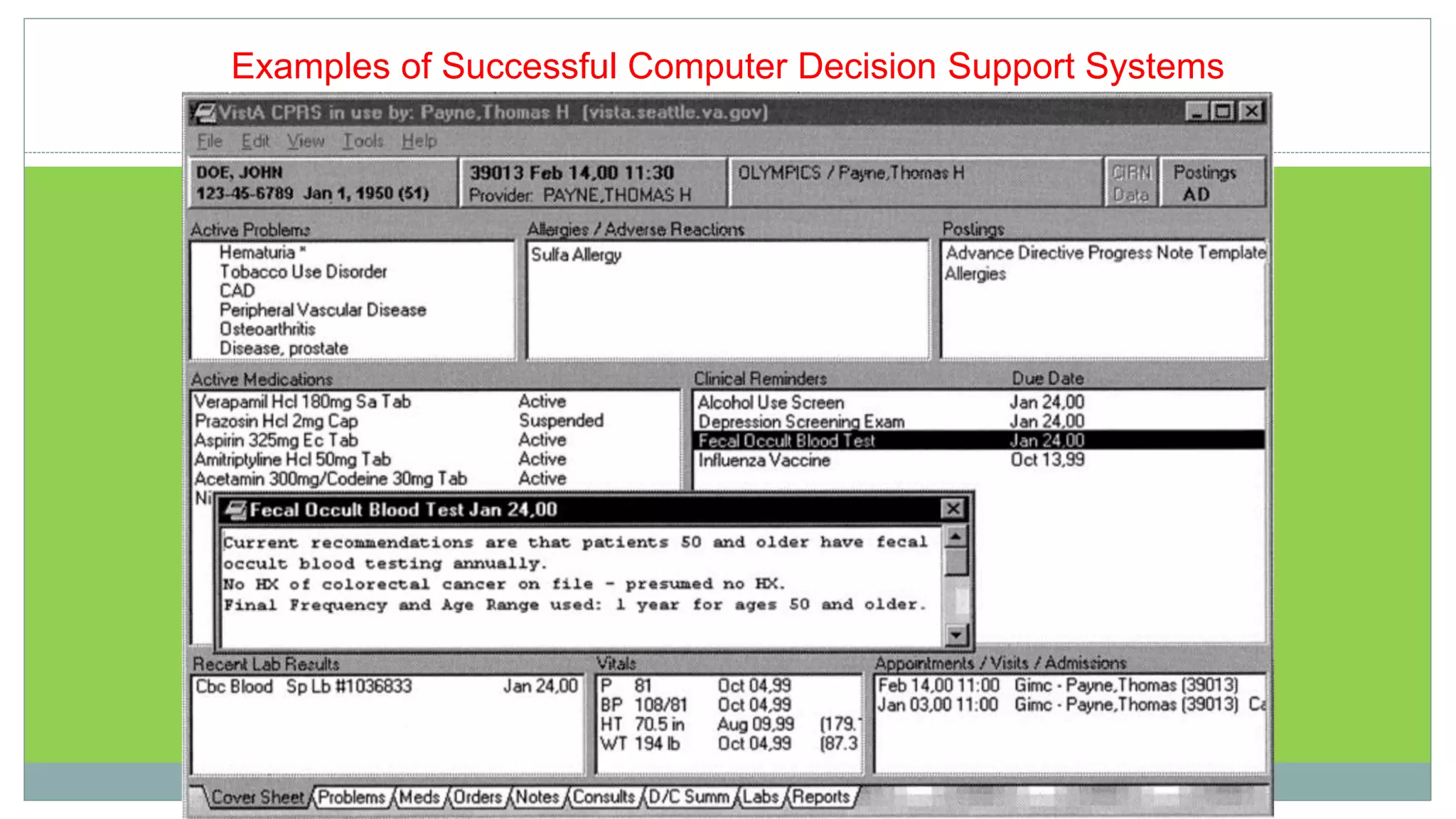
This document defines clinical decision support systems (CDSS) and outlines their key components and challenges. It begins by defining CDSS as computer programs that help health professionals make clinical decisions. It then describes the main categories of CDSS, including diagnostic assistance, therapy planning, and image recognition. The document outlines the typical system architecture of CDSS including tools for information management, focusing attention, and patient-specific consultation. It also discusses the need for CDSS, potential applications, disadvantages, and challenges to implementation. Throughout, it provides examples to illustrate different types of CDSS.