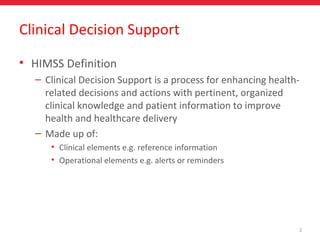
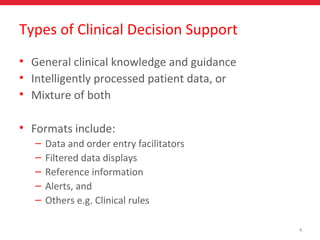
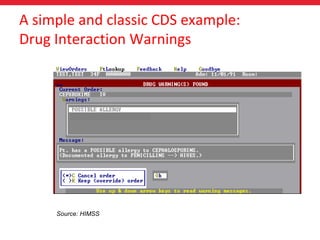
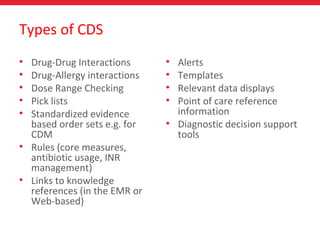
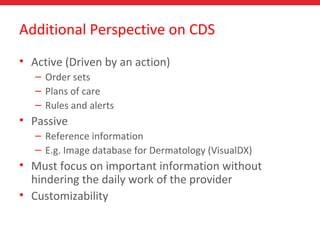
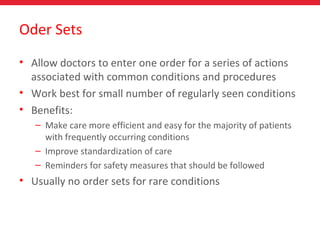
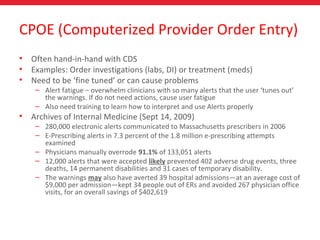
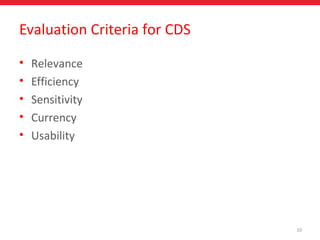
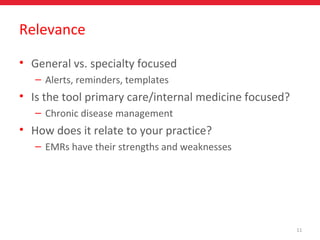
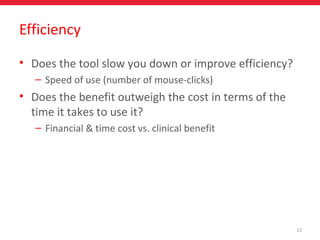
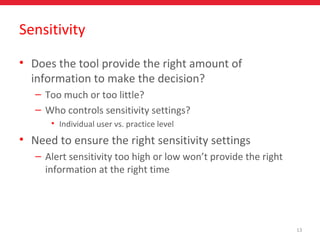
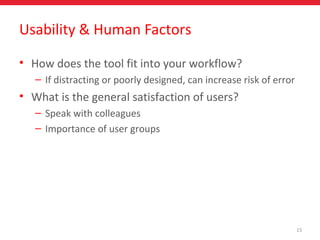
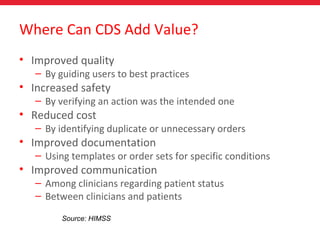
The document discusses clinical decision support (CDS) systems, which enhance healthcare-related decisions with organized clinical knowledge and patient information. It covers types of CDS, including alerts for drug interactions and dose checking, and emphasizes the importance of usability and integration within clinical workflows. Additionally, it highlights that effective CDS can improve patient care quality, safety, documentation, and communication, while also warning against issues like alert fatigue.