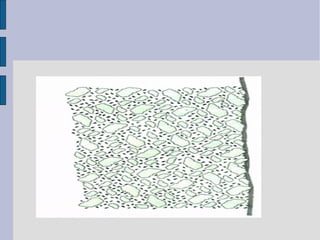
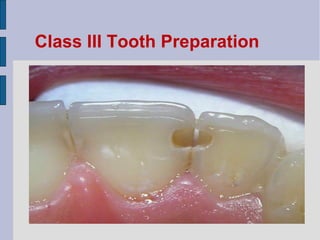
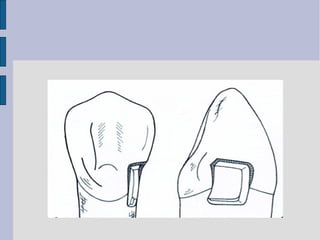
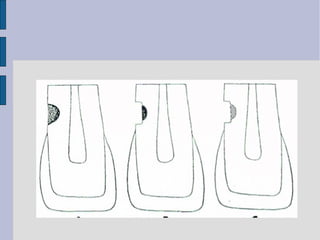
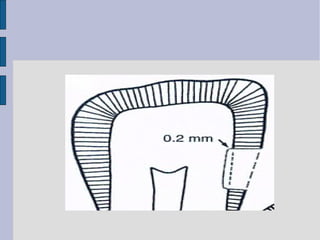
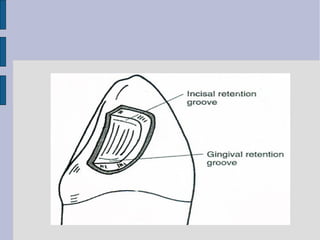
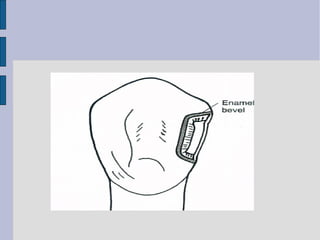
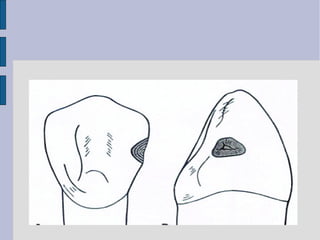
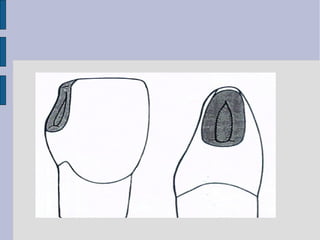
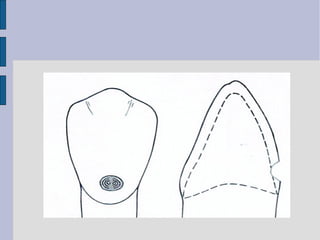
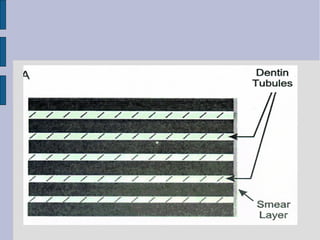
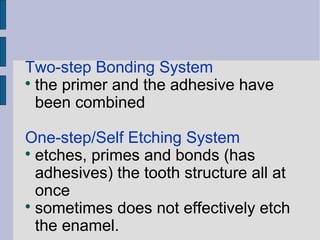
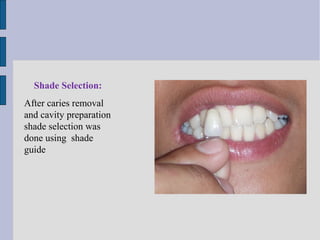
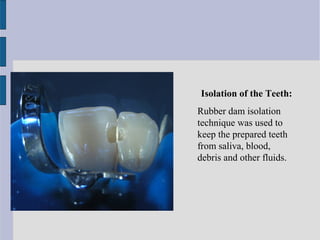
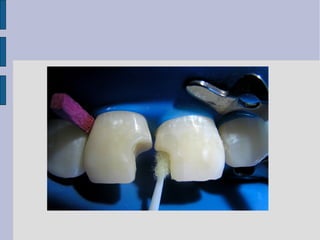
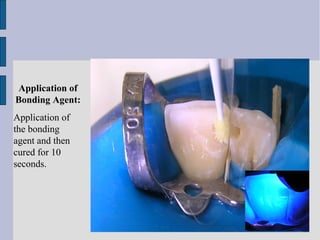
The document provides detailed information on direct composite restorations, including indications, contraindications, advantages, and disadvantages of various types, such as conventional, microfilled, hybrid, flowable, and packable composites. It outlines clinical techniques for class III, IV, and V restorations, detailing tooth preparation methods and entry approaches. Key features of nanocomposites and their enhanced properties due to nanoparticulates are also discussed.