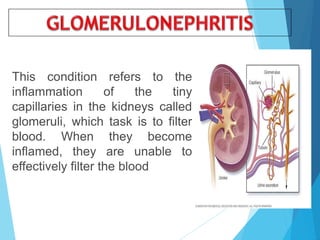
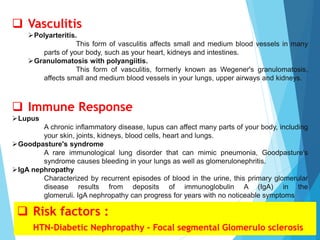
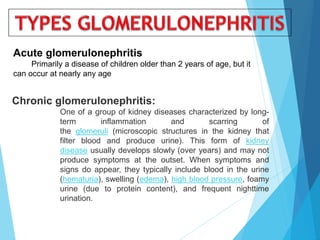
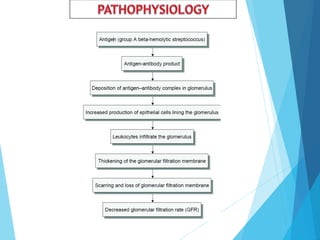
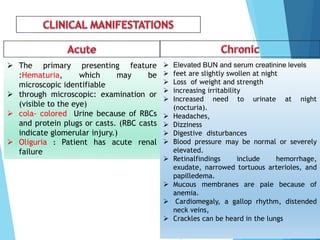
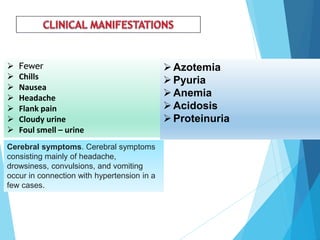
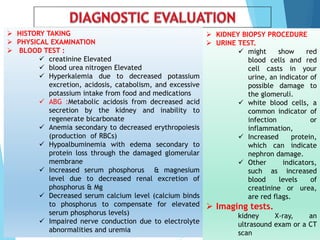
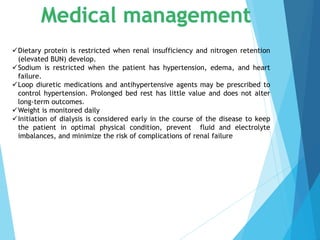
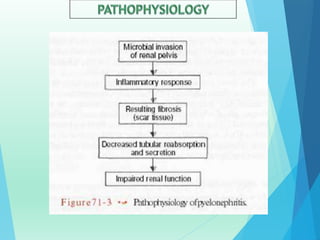
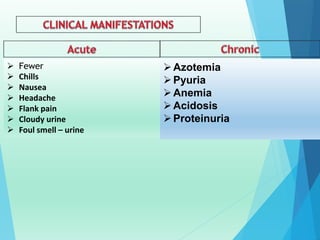
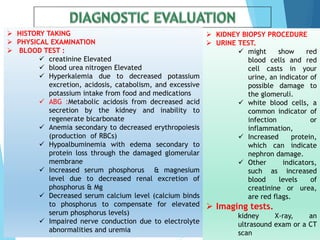
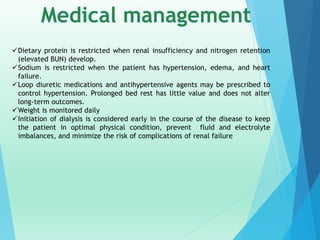
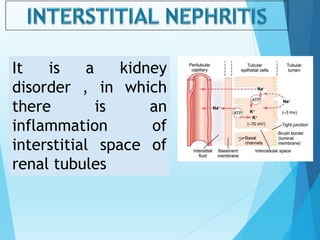
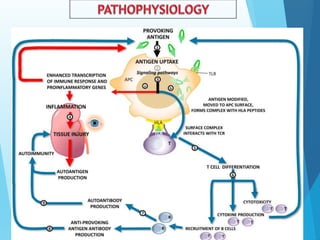
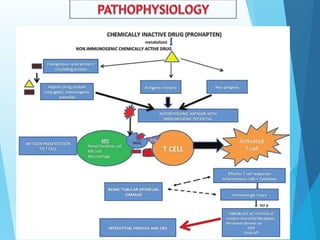
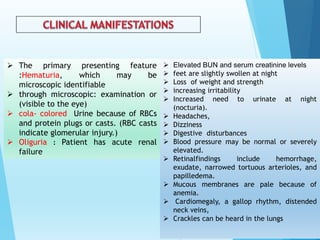
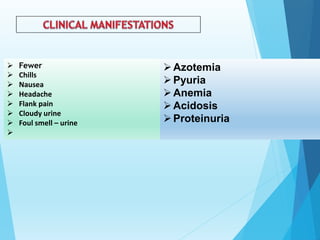
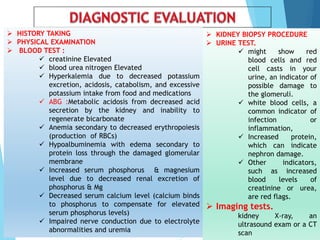
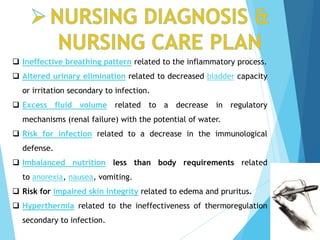
Nephritis refers to inflammation of the kidneys that can be caused by various factors like infection, autoimmune disease, or kidney disease. It affects the glomeruli, tubules, or surrounding tissue and can lead to impaired kidney function. Symptoms vary depending on the specific type and cause of nephritis but may include blood or protein in the urine, high blood pressure, swelling, and changes in kidney function test results. Treatment involves addressing the underlying cause, managing complications, and potentially using medications, dietary changes, or dialysis.