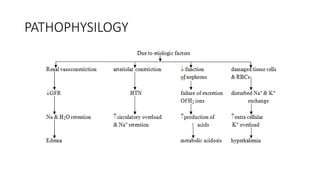
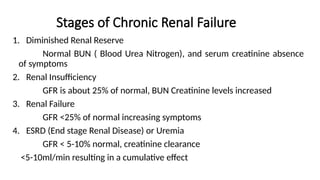
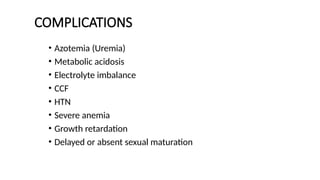
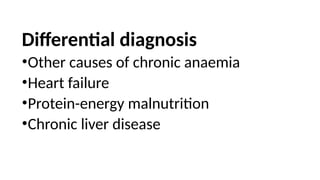
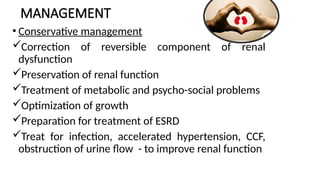
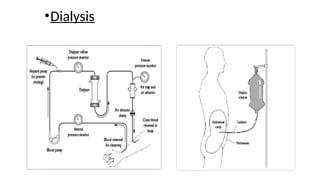
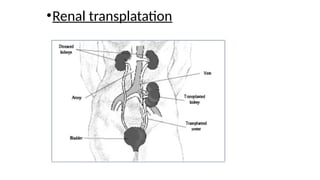
Renal failure is a condition where kidneys lose their ability to filter waste and maintain balance of fluids and electrolytes, classified into acute renal failure (ARF) and chronic renal failure (CRF). ARF can be reversible and is caused by prerenal, intrinsic, or postrenal factors, while CRF leads to permanent damage and is often due to conditions like diabetes and hypertension. Management includes treating underlying causes, dietary modifications, and monitoring, with potential dialysis for severe cases.