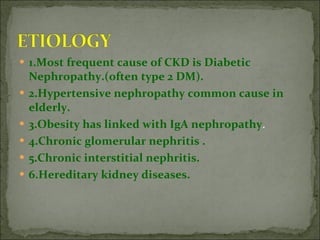
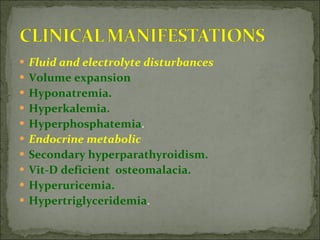
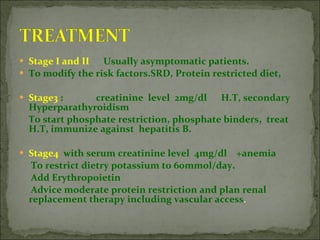
The document discusses chronic kidney disease (CKD), defining it as kidney damage or decreased kidney function for more than 3 months. It stages CKD based on glomerular filtration rate (GFR) and describes risk factors, complications, diagnostic tests, and treatment approaches based on CKD stage. The primary goals of treatment are slowing progression and managing complications through modifying risk factors, medical therapy, and preparing for renal replacement therapy if needed.