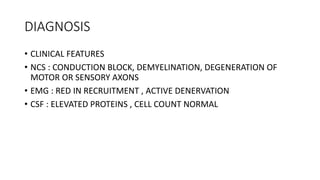
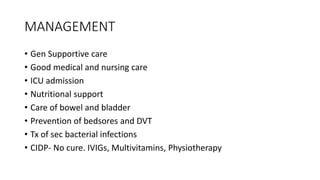
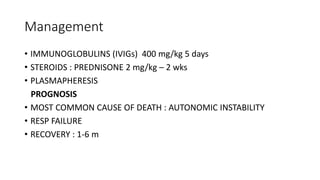
This document discusses chronic inflammatory demyelinating polyneuropathy (CIDP), Guillain-Barré syndrome (GBS), and post-polio syndrome. CIDP is a neurological disorder involving progressive weakness and reduced sensation. GBS is an acute inflammatory polyneuropathy and the most common cause of acute flaccid paralysis. It presents with symmetrical weakness and loss of reflexes. Post-polio syndrome causes muscle pain and new or exacerbated weaknesses in people who had polio decades prior. Management of these conditions includes immunoglobulins, steroids, physical therapy, and lifestyle modifications.