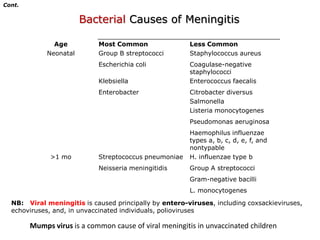
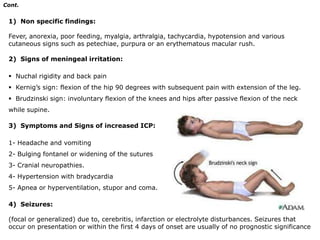
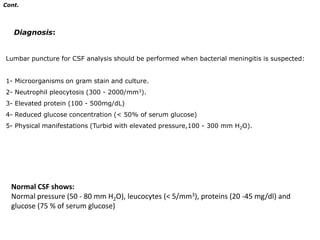
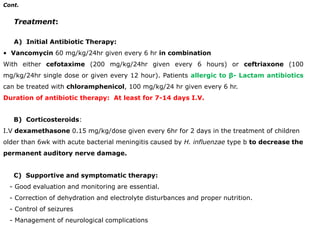
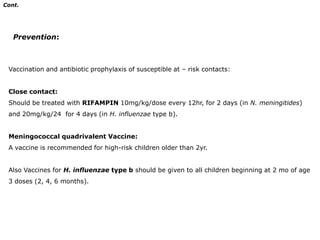
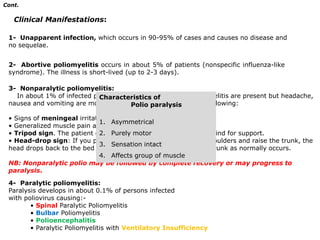
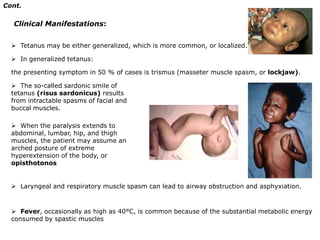
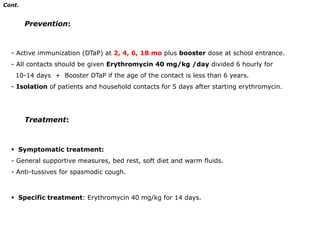
This document discusses several infectious diseases, including meningitis, encephalitis, poliomyelitis, mumps, tetanus neonatorum, and pertussis. It describes the etiology, clinical manifestations, diagnosis, and treatment of each disease. Meningitis can be caused by bacteria, viruses, or fungi and symptoms include fever, headache, and neck stiffness. Encephalitis is usually caused by viruses and may cause seizures, behavioral changes, and neurological deficits. Poliomyelitis is caused by polioviruses and can cause flu-like symptoms or potentially paralysis.