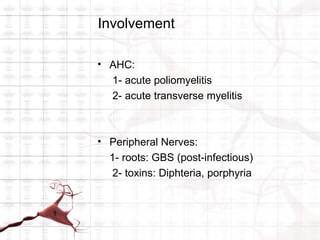
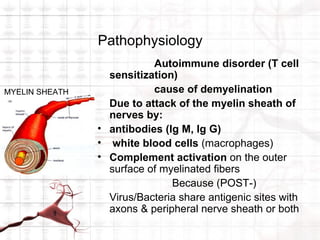
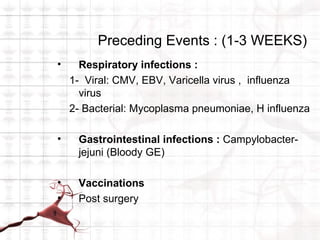
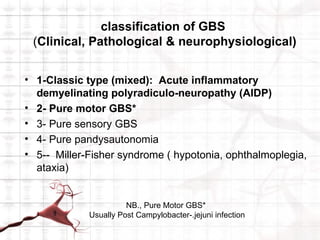
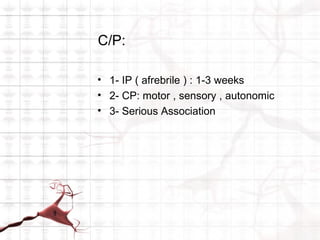
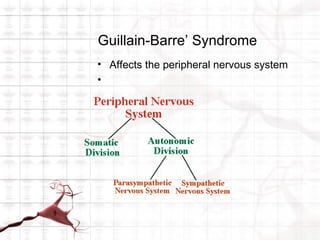
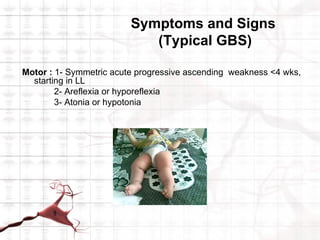
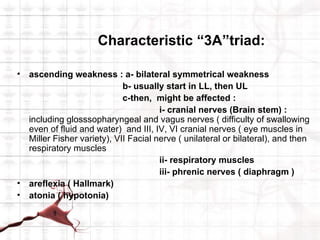
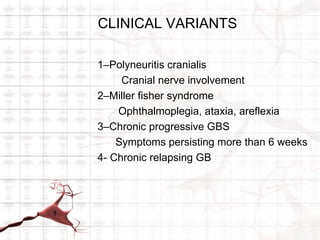
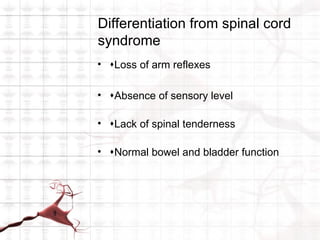
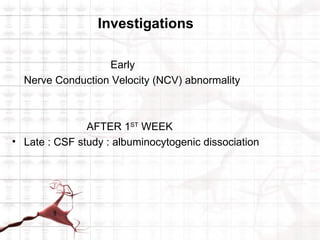
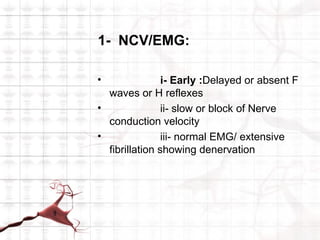
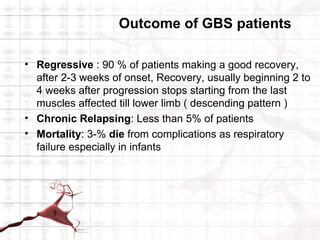
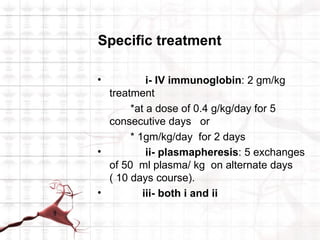
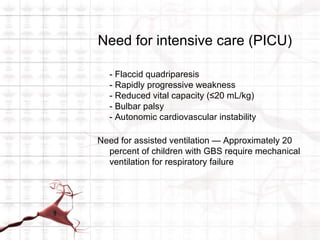
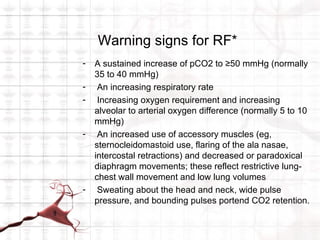
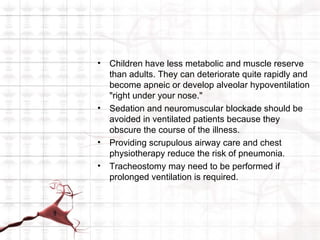
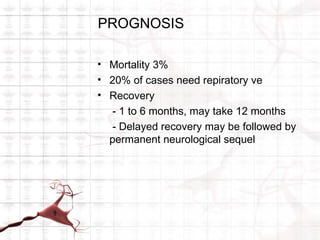
Guillain-Barré syndrome (GBS) is the most common cause of acute flaccid paralysis among infants. It is an autoimmune disorder that causes acute, rapidly progressive, and potentially fatal paralysis. The classic presentation involves ascending symmetric motor weakness, areflexia, and ataxia. Treatment involves hospitalization, IV immunoglobulin, plasmapheresis, and supportive care including ventilation if needed. Most patients recover fully but some have residual deficits and rare cases are chronic or fatal.