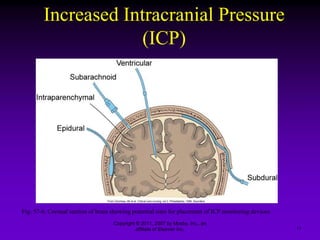
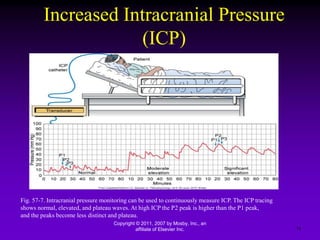
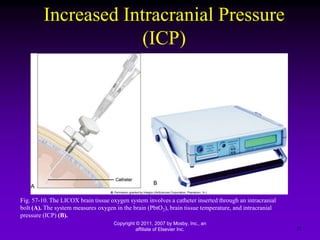
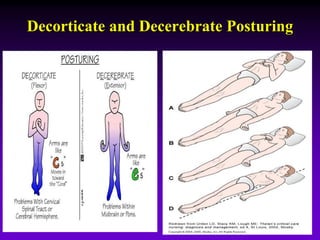
This document discusses nursing management of intracranial pressure. It begins by defining intracranial pressure and factors that can influence it such as brain volume, blood volume, cerebrospinal fluid volume, arterial pressure, venous pressure and more. Signs of increased intracranial pressure include changes in vital signs, decreased motor function, headache and vomiting. Nursing goals for management include maintaining normal intracranial pressure, airway, fluid/electrolyte balance and positioning the patient appropriately. Interventions discussed include medication administration, oxygen therapy, monitoring devices, drainage of cerebrospinal fluid and maintaining proper nutrition.