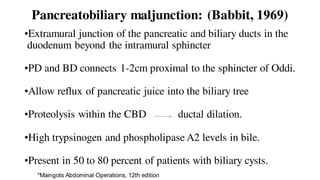
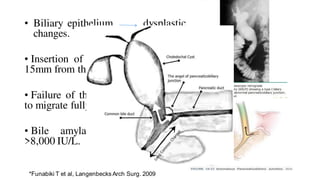
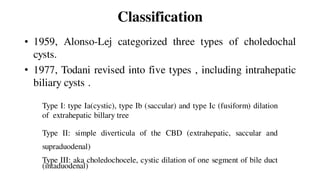
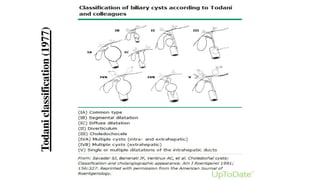
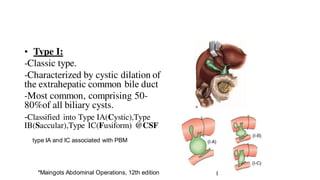
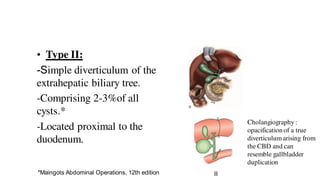
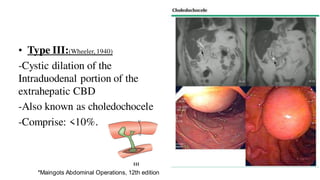
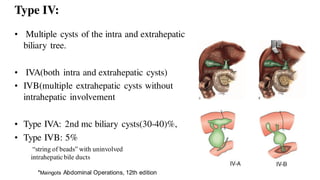
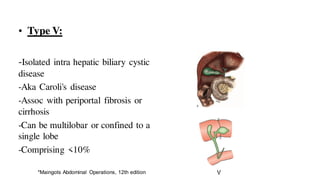
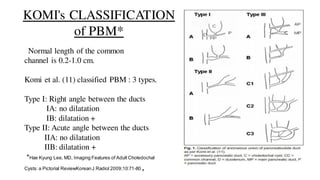
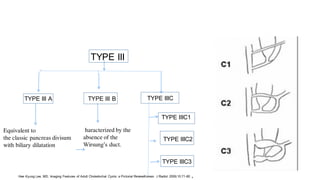
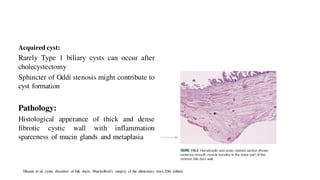
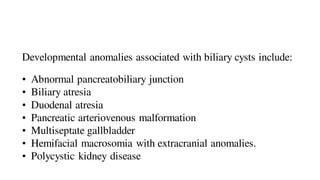
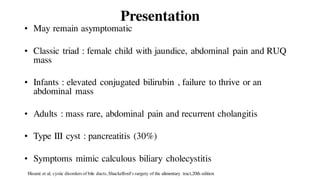
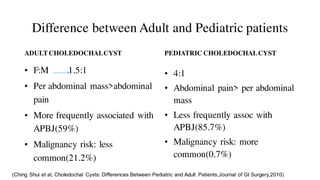
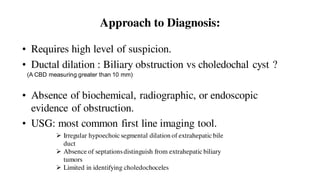
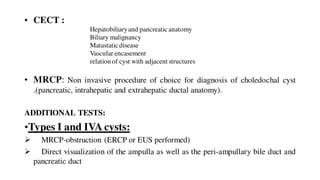
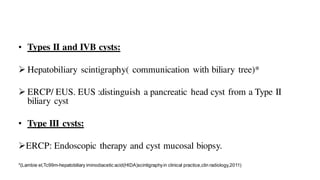
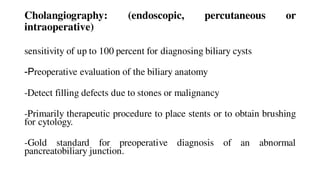
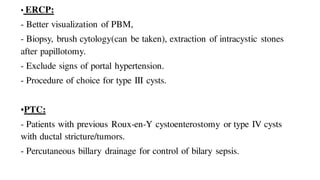
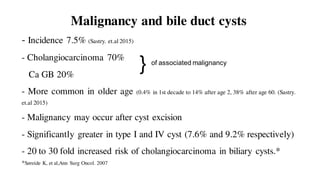
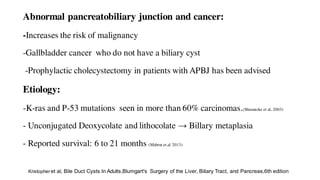
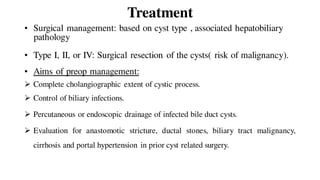
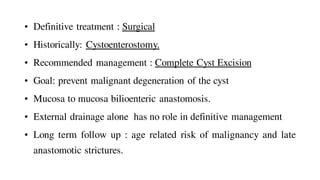
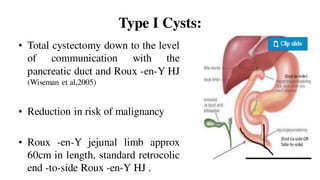
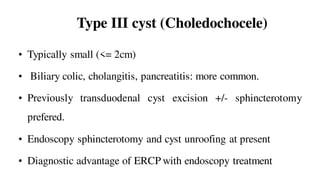
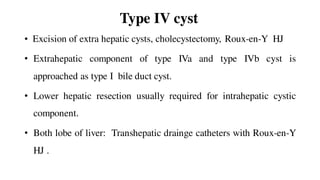
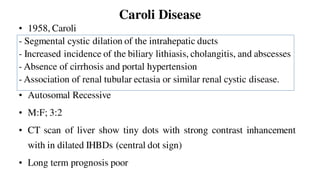
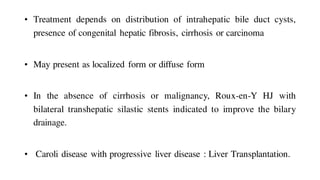
Choledochal cysts are rare, usually diagnosed in children and involve pathological dilatation of the biliary system. They are classified into 5 types based on location and appearance. Type 1 cysts involve the extrahepatic bile duct and are the most common. Diagnosis involves imaging like ultrasound, CT, MRCP and sometimes cholangiography. Treatment is complete surgical excision to prevent malignancy, with Roux-en-Y hepaticojejunostomy for biliary reconstruction. Long term follow up is needed due to risk of malignancy and anastomotic strictures.