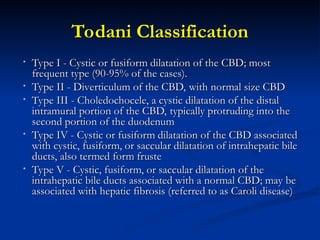
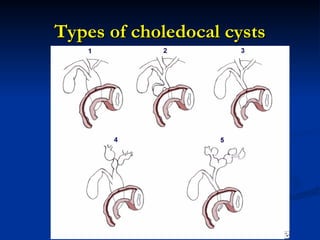
Choledochal cysts are congenital anomalies of the bile ducts, occurring in approximately 1 in 10,000 to 13,000 live births, and are more prevalent in women and Asians. They are classified into five types according to Todani's classification, with Type I being the most common. Complications include pancreatitis, cholangitis, and an increased risk of cholangiocarcinoma, with treatment options varying based on the type of cyst.