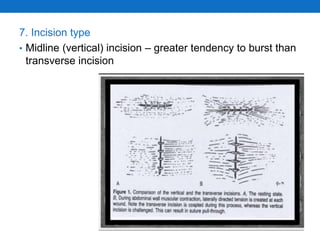
Burst abdomen, or postoperative separation of an abdominal wound, occurs most commonly between the 5th and 8th postoperative days when wound strength is weakest. It can be partial or complete, and risk factors include preexisting malnutrition or disease, operative issues like poor technique or closure, and post-operative infections. Treatment depends on severity but may involve reapproximating the wound with sutures or a temporary dressing, with prevention prioritizing proper technique, antibiotics, and minimizing intra-abdominal pressure increases.