Choledochal cysts are rare biliary system dilations, common in Asian populations and often presenting in infancy. Diagnosis is critical due to associated risks like cholangitis and malignancy, and various imaging methods such as ultrasound and CT scans are utilized for identification. Management typically involves surgical resection and reconstruction, with specific approaches depending on the cyst type.
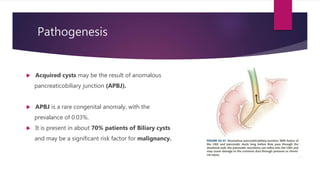

![Cholangiography
Direct cholangiography (whether intraoperative, percutaneous or endoscopic) has
a sensitivity of up to100% for diagnosing biliary cysts and previously was a
commonly obtained test.
Can identify abnormal pancreatobiliary junction and filling defects due to stones
or malignancy.
Increase risk of cholangitis and pancreatitis. [Patients with cystic disease are
greater risk for these complications]](https://image.slidesharecdn.com/choledochalcyst-190917153706/85/Choledochal-cyst-13-320.jpg)
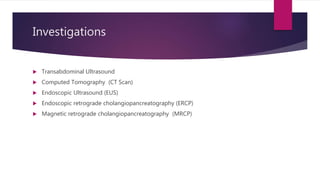
![Magnetic resonance
cholangiopancreatography (MRCP)
Does not have the risks of cholangitis and pancreatitis as direct cholangiography.
Sensitivity 73 – 100%
Less sensitive than direct cholangiography for excluding obstruction.
The data are variable with regard to its ability to diagnose an abnormal
pancreatobiliary junction. [46-75%]](https://image.slidesharecdn.com/choledochalcyst-190917153706/85/Choledochal-cyst-14-320.jpg)