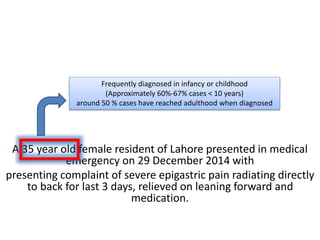
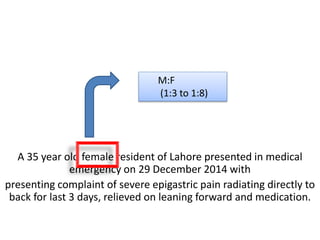
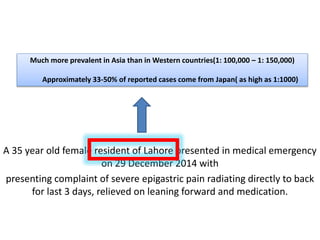
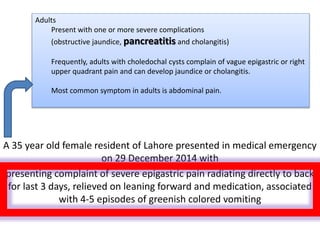
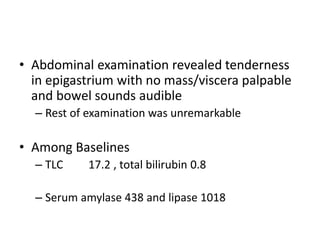
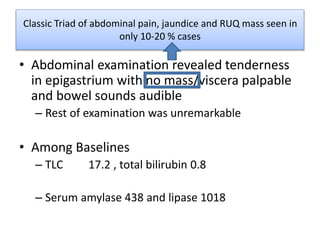
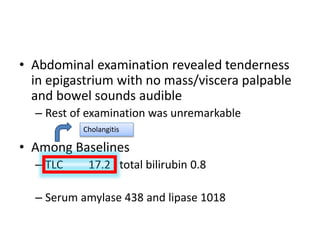
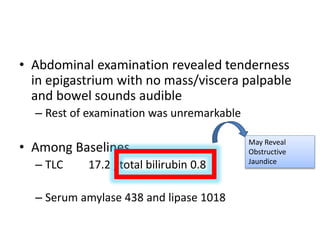
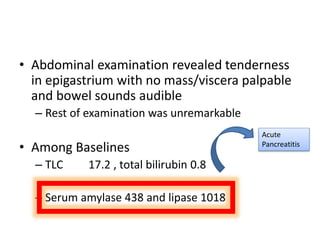
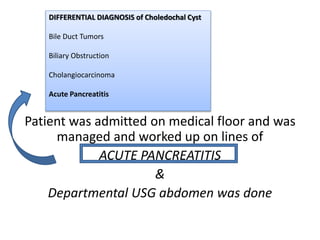
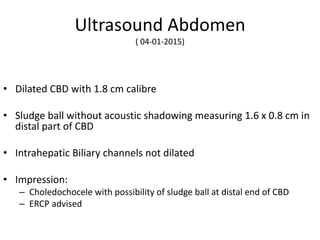
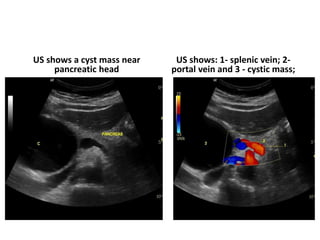
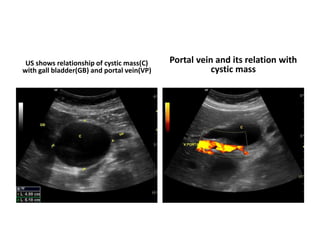
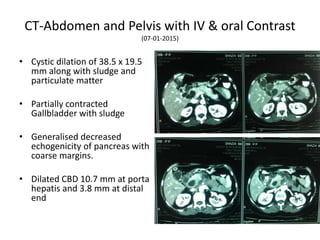
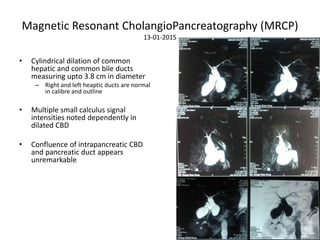
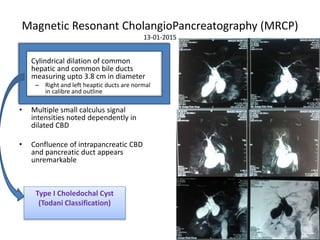
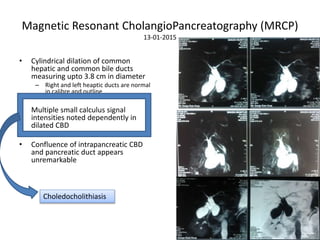
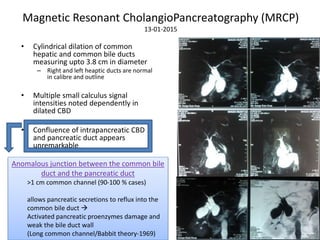
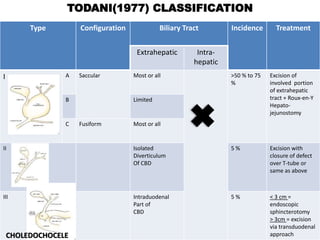
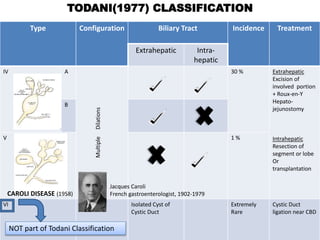
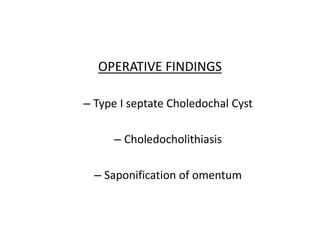
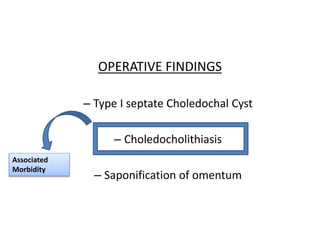
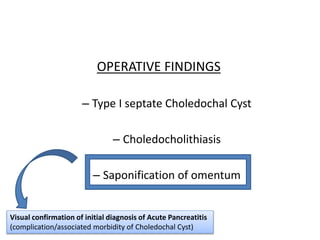
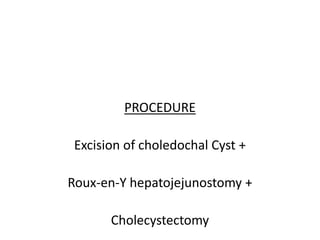
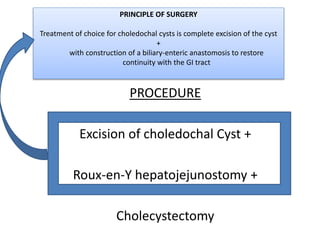
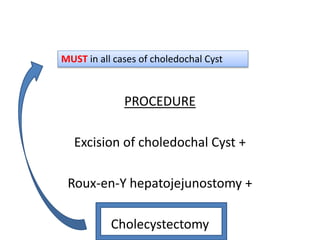
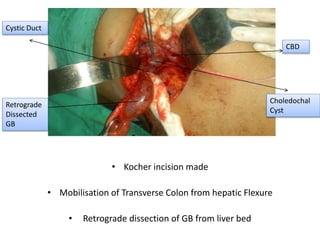
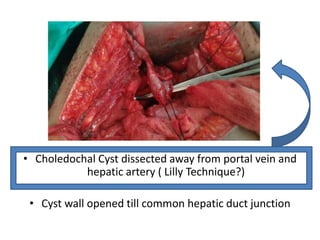
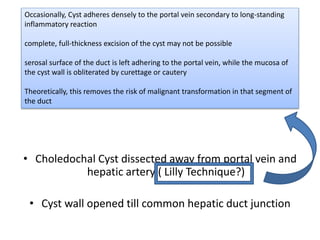
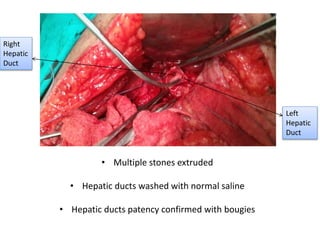
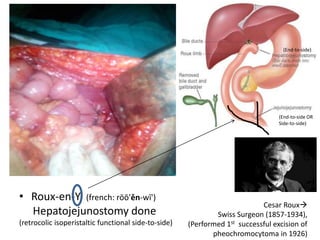
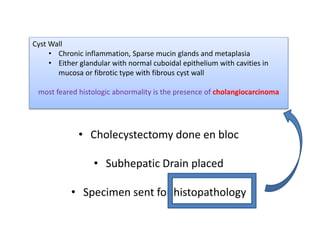
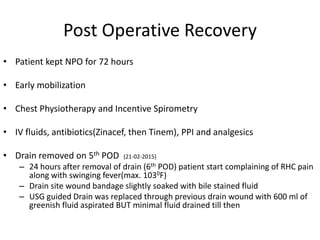
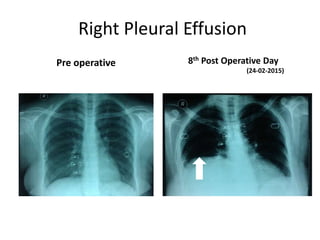
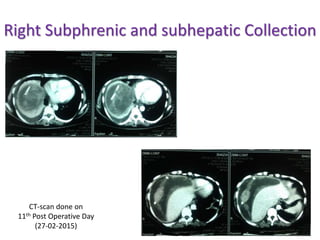
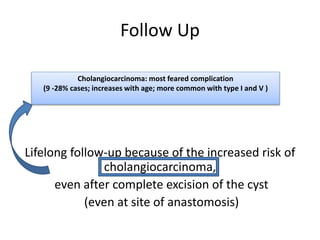
A 35-year-old female presented with severe epigastric pain indicative of a choledochal cyst, which is more prevalent in Asia. Diagnostic imaging revealed type I choledochal cyst along with choledocholithiasis, leading to surgical intervention involving excision and biliary reconstruction. Post-operative recovery included monitoring for complications, with emphasis on lifelong follow-up due to increased risk of cholangiocarcinoma.