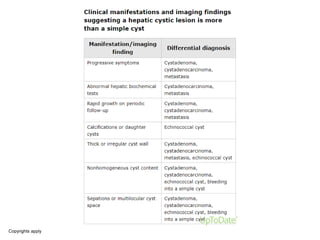
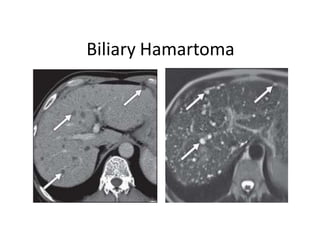
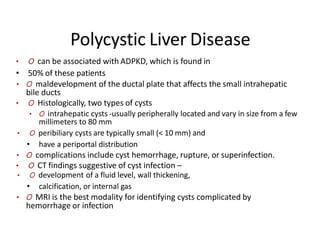
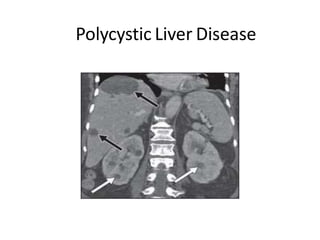
The document discusses the diagnosis and treatment of cystic lesions of the liver. It outlines various types of cysts that can occur in the liver including simple cysts, biliary hamartomas, Caroli disease, polycystic liver disease, and others. For each type, it describes the imaging appearance on ultrasound, CT, and MRI. Key diagnostic features are discussed to help differentiate benign from malignant cysts. An algorithm is proposed for approaching the diagnosis of cystic liver lesions based on clinical history and imaging characteristics. Definitive diagnosis or differential diagnosis can be established to guide appropriate patient management.