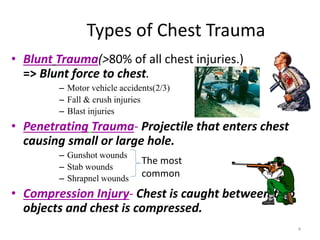
1) Chest trauma is a common cause of injury and death, especially from road traffic accidents, gunshot wounds, and falls.
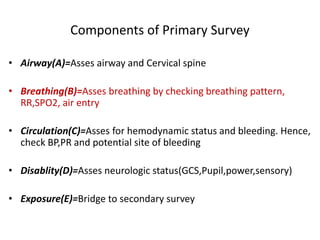
2) The initial evaluation and resuscitation of chest trauma patients follows the ATLS protocol, assessing the ABCDEs: Airway, Breathing, Circulation, Disability, and Exposure.
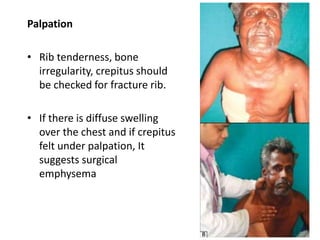
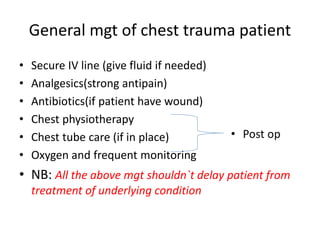
3) Common chest injuries include pneumothorax, hemothorax, and flail chest. Tension pneumothorax requires immediate needle decompression. Management involves chest tube placement, oxygen, monitoring, and treatment of underlying conditions.