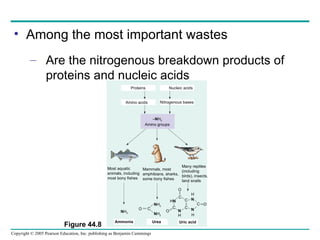
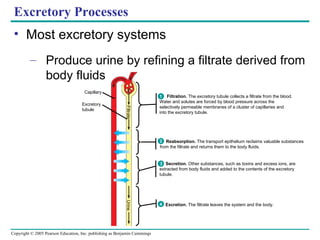
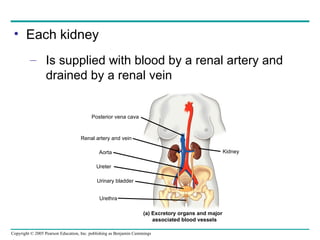
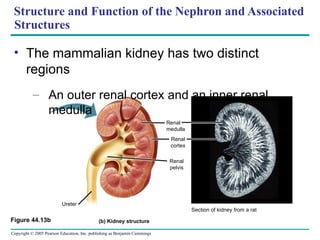
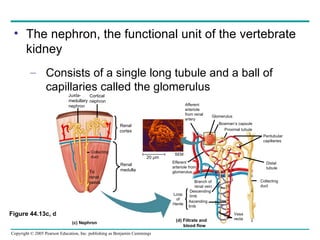
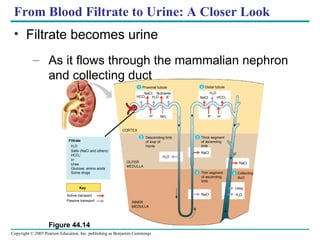
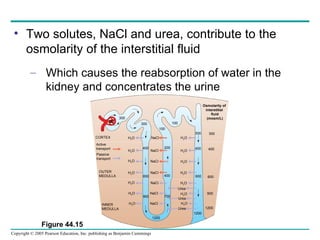
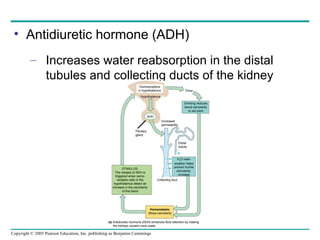
The document discusses homeostasis and osmoregulation in animals. It explains that animals must maintain fairly narrow concentrations of water and solutes. It then describes different mechanisms that aquatic, desert, and marine animals use for osmoregulation. These include adaptations for water uptake, conservation of solutes, and regulation of water and solute balance between internal fluids and the external environment. The document also discusses the roles of the kidneys, nephrons, and associated structures in vertebrate osmoregulation and excretion.