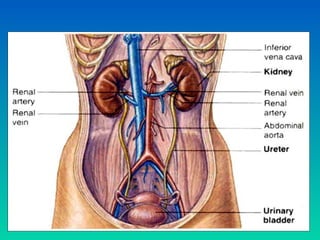
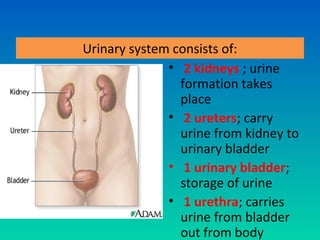
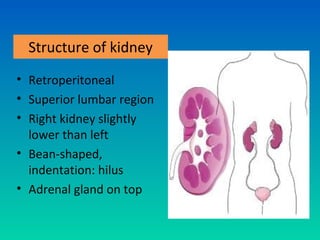
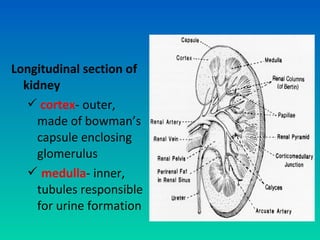
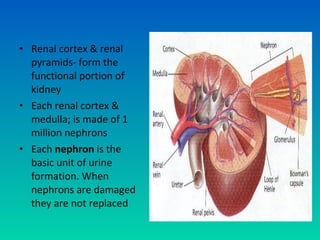
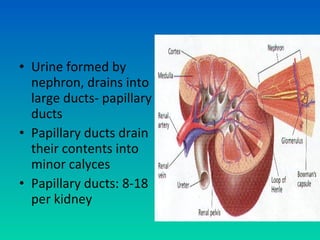
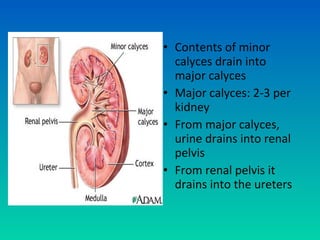
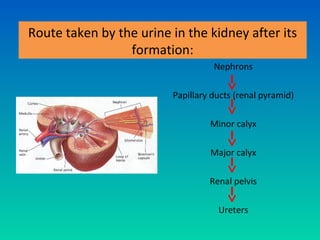
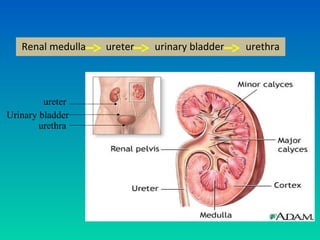
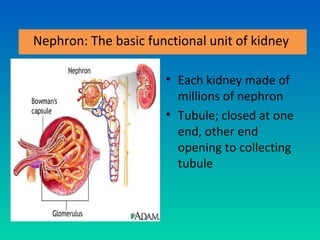
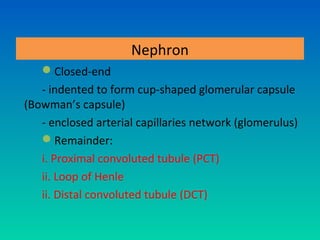
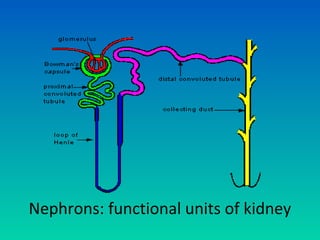
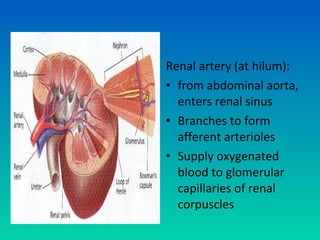
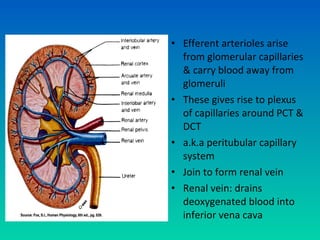
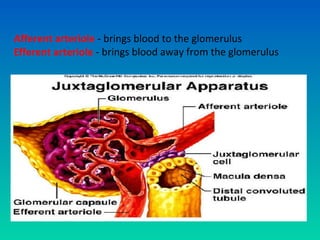
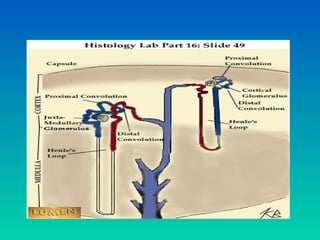
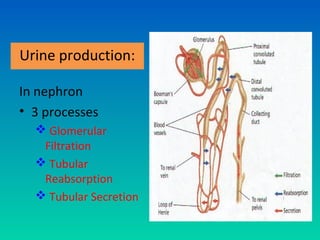
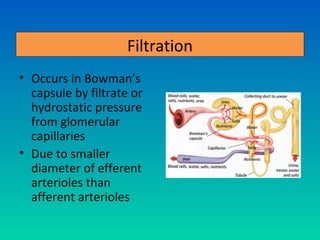
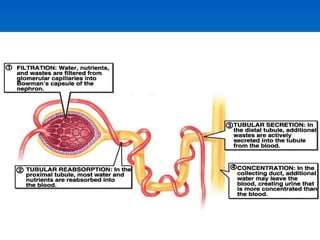
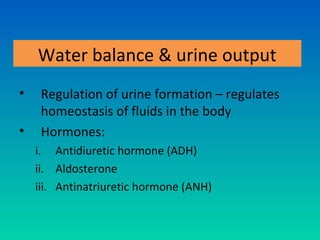
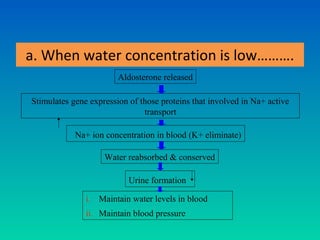
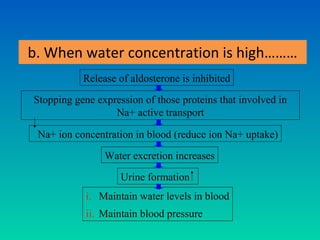
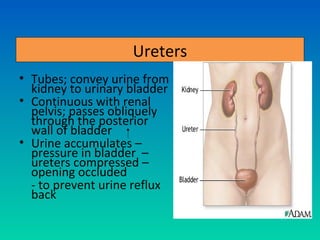
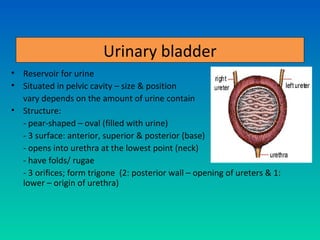
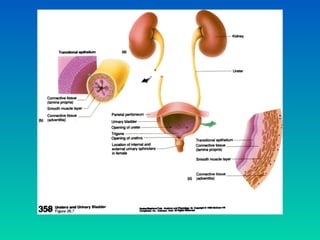
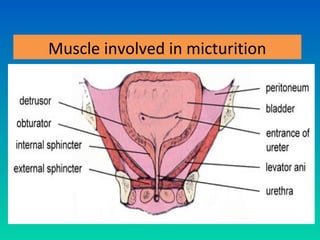
The urinary system consists of the kidneys, ureters, urinary bladder, and urethra. The kidneys filter waste from the blood to form urine. Each kidney contains over 1 million nephrons, the basic functional units that filter blood and form urine. Urine travels from the kidneys through the ureters to the urinary bladder, where it is stored until micturition. During micturition, muscles contract to expel urine through the urethra and out of the body. Precise regulation of urine production, composition, and excretion helps maintain fluid and electrolyte balance in the body.