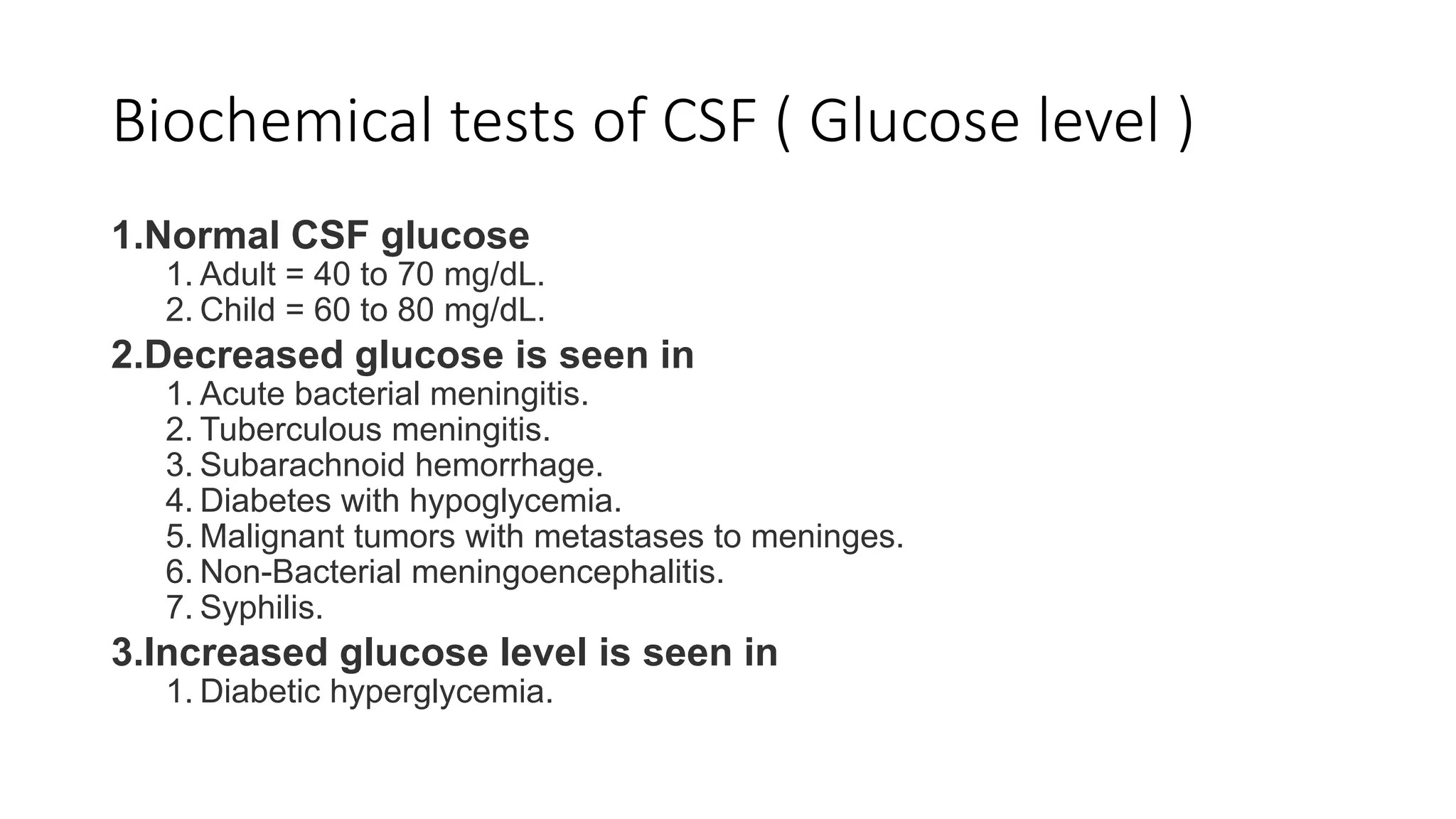
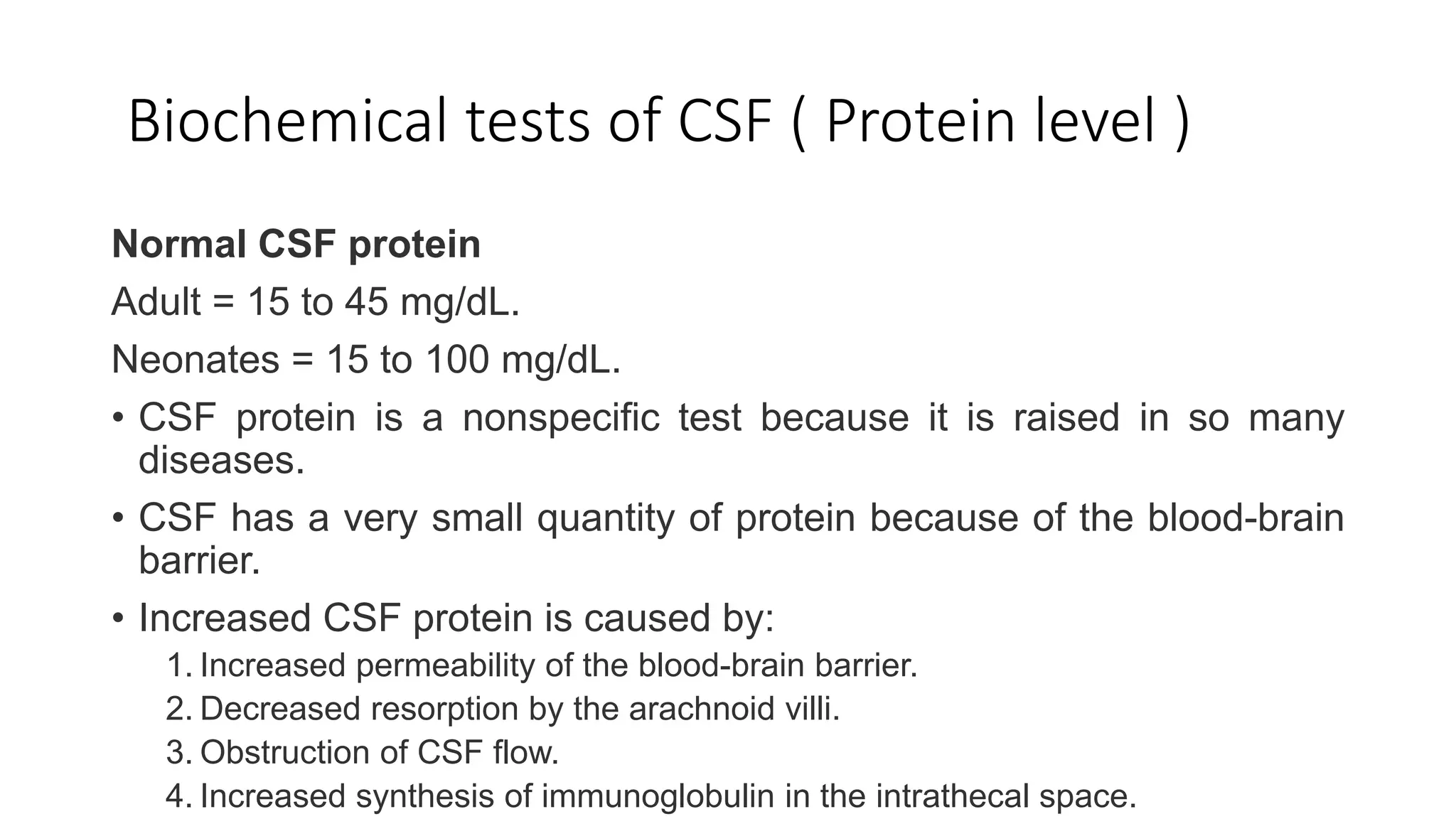
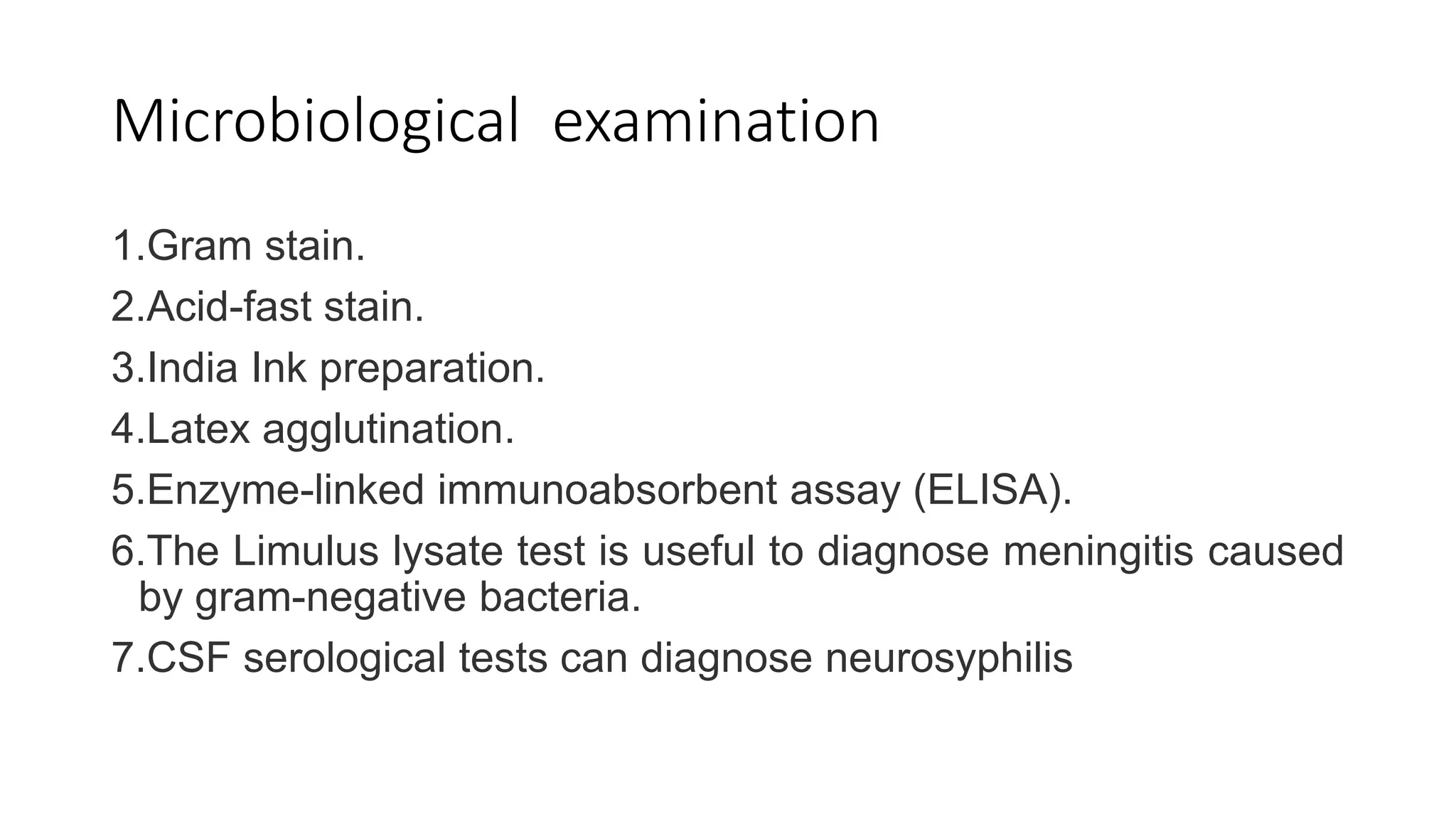
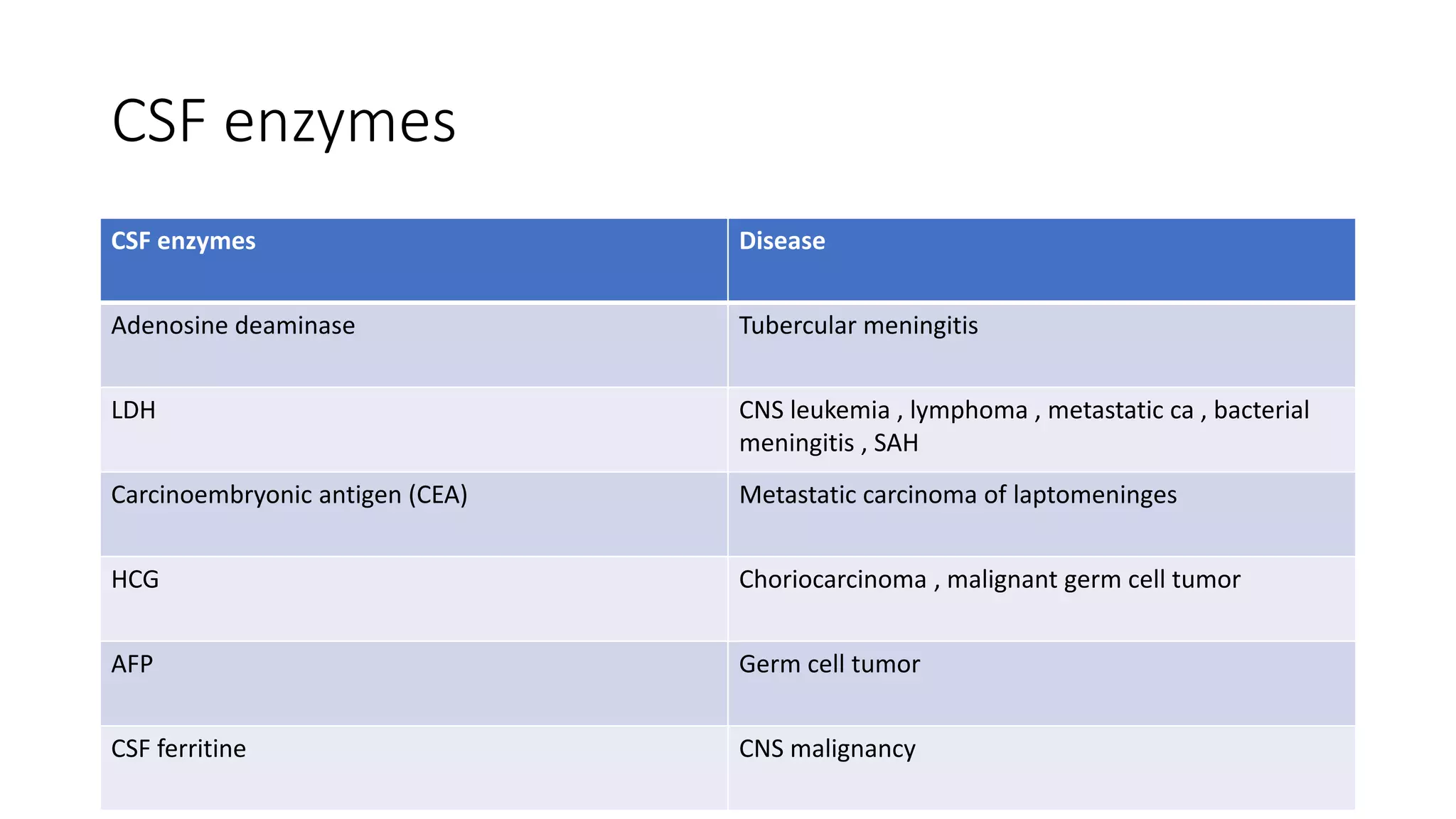
CSF analysis provides important diagnostic information for diseases of the central nervous system. CSF is produced by the choroid plexus at a rate of 550 ml per day and its functions include removing waste, circulating nutrients, and cushioning the CNS. Laboratory examination of CSF includes physical, biochemical, microscopic, and microbiological analyses. Physical examination evaluates features like volume, appearance, color, pH and specific gravity. Biochemical tests measure glucose and protein levels which can indicate infections, inflammation or tumors. Microscopic examination identifies cell counts and types which are diagnostic for conditions like bacterial meningitis. Microbiological tests include gram stain, culture and sensitivity to identify infectious organisms. Together these analyses of CSF properties and components aid in diagnosis of CNS