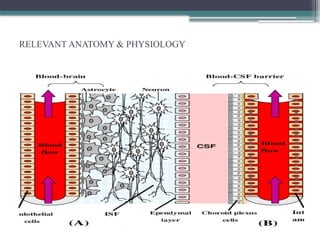
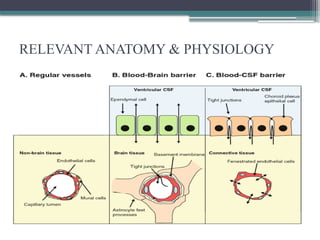
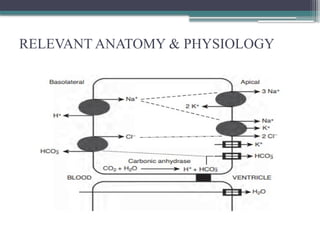
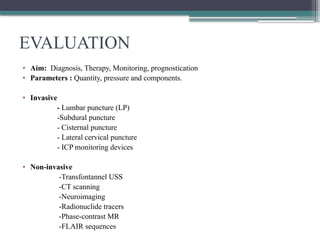
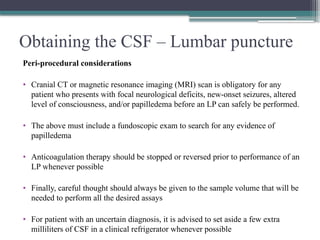
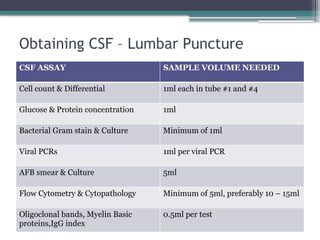
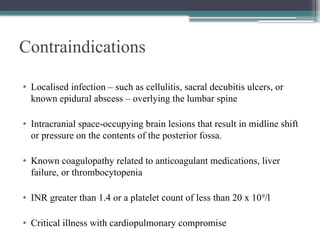
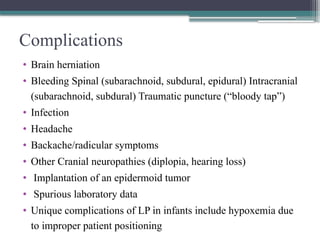
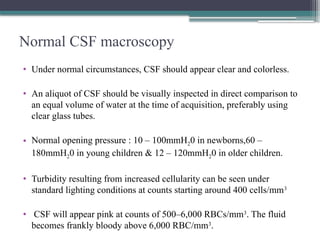
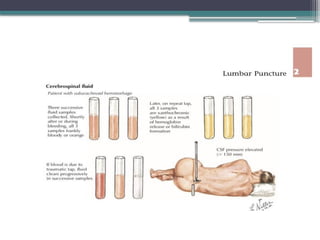
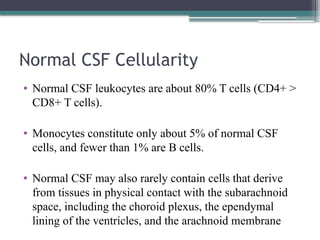
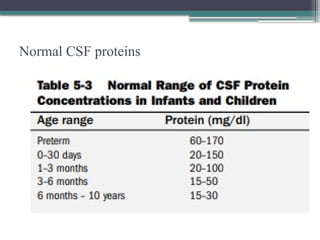
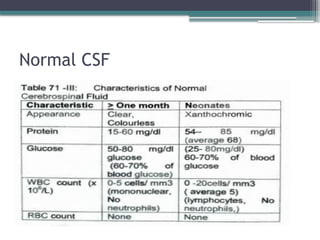
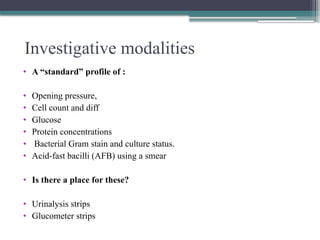
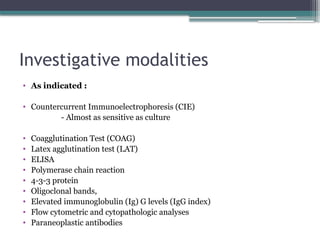
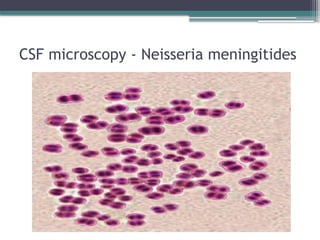
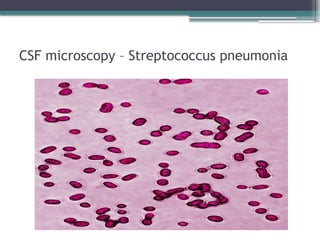
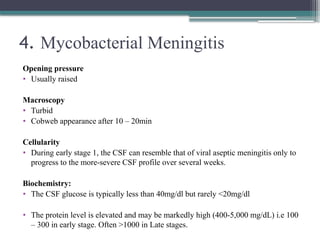
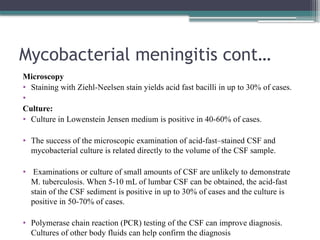
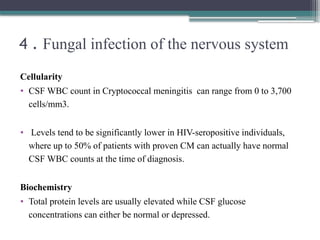
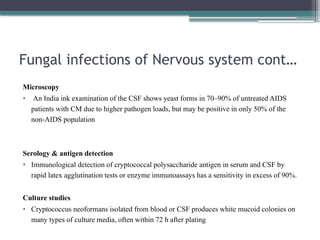
The document provides a comprehensive overview of the diagnostic evaluation of cerebrospinal fluid (CSF), detailing its historical background, anatomy, and the procedures for obtaining and analyzing CSF. It emphasizes the importance of CSF analysis as a vital tool for diagnosing various neurological disorders and outlines specific findings associated with conditions such as bacterial and viral meningitis, mycobacterial meningitis, and other neurological infections. Additionally, it highlights the complications and precautions associated with lumbar punctures and the evolving investigative modalities in CSF diagnostics.