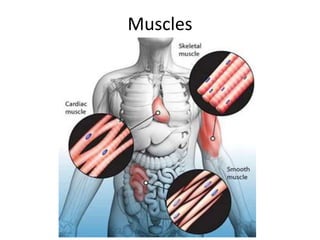
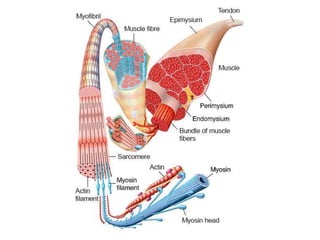
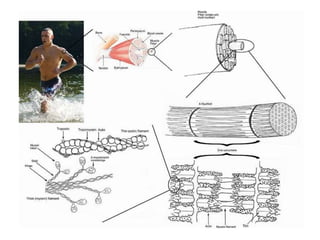
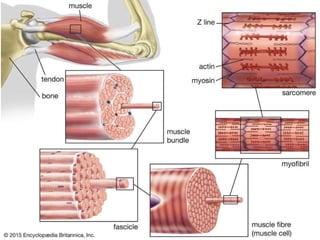
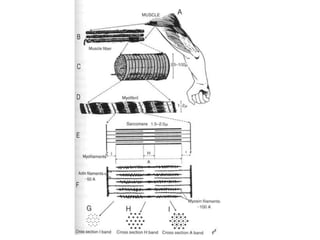
- There are three main types of muscle in the body: cardiac, smooth, and skeletal.
- Cardiac muscle is only found in the heart and contracts involuntarily. Smooth muscle lines internal organs and contracts slowly and rhythmically for involuntary functions. Skeletal muscle is striated and attached to bones, allowing voluntary movement.
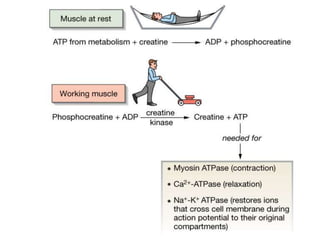
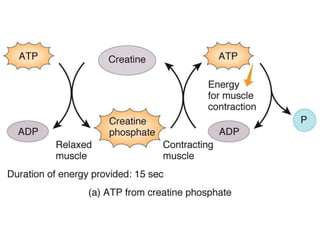
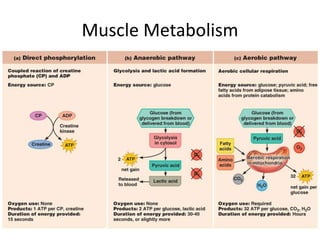
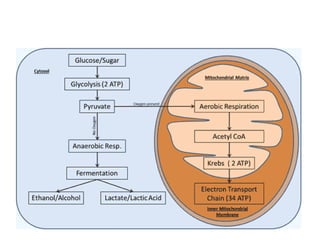
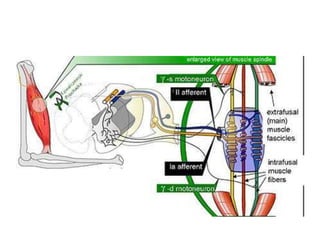
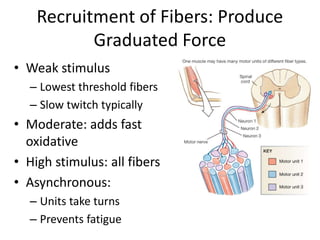
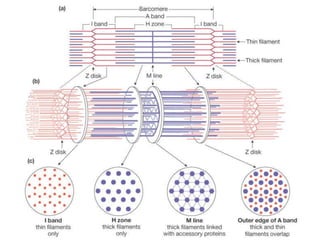
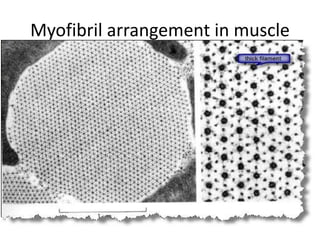
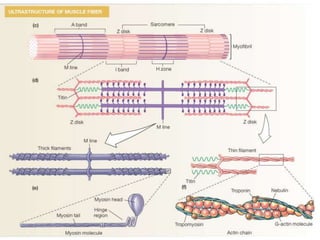
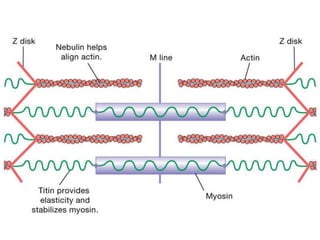
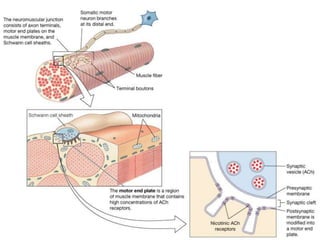
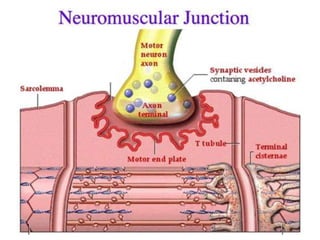
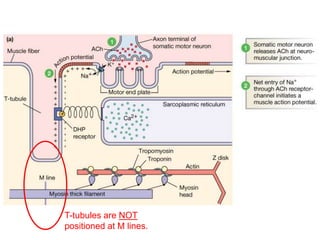
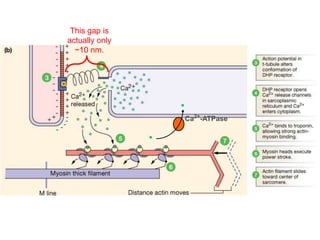
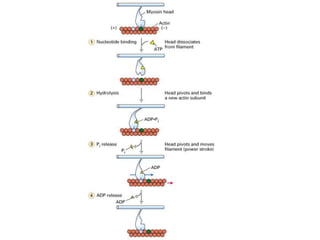
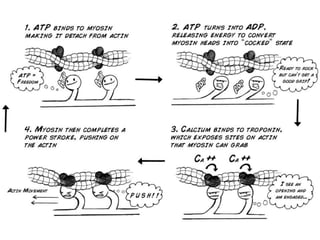
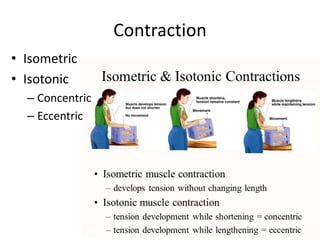
- Muscle contraction occurs through a complex process involving motor neurons, calcium ions, actin and myosin filaments, and ATP. Proper hydration, electrolyte balance, exercise, and diet can help prevent muscle cramps. Stretching muscles regularly promotes flexibility and reduces cramping.



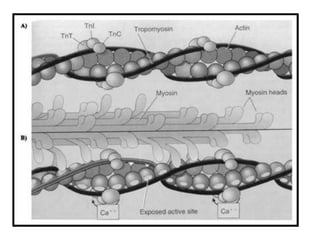
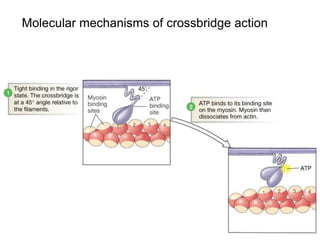
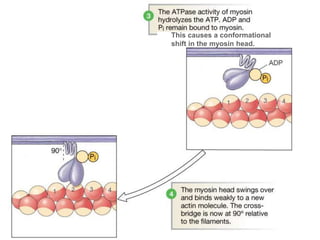
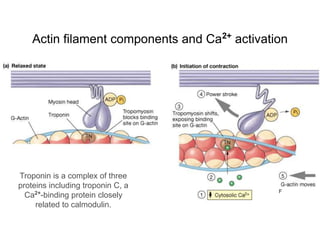
![Binding of myosin to actin
leads to release of Pi.
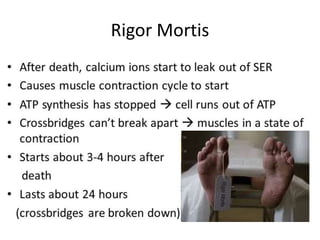
After death, as ATP runs out,
cytosolic [Ca2+
] slowly rises,
actin binding sites are opened,
crossbridges are formed and
become locked in the "rigor"
position without ATP to bind.](https://image.slidesharecdn.com/cellphysiology2-201006142544/85/Cell-physiology2-32-320.jpg)

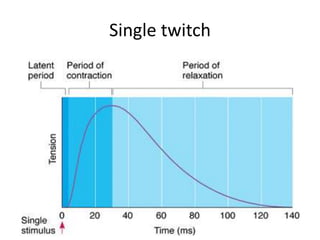

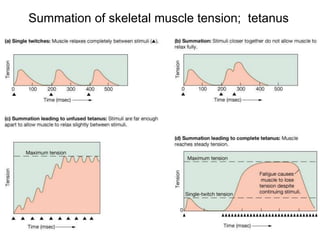
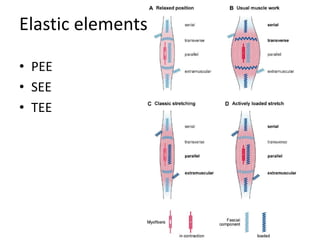
![Time is required for maximal twitch force to develop, because some
shortening of sarcomeres must occur to stretch elastic elements of
muscle before force can be transmitted through tendons
By the time this maximal force is developed, [Ca2+
] and number of
active crossbridges have greatly decreased, so an individual twitch
reaches much less than the maximum force the muscle can develop](https://image.slidesharecdn.com/cellphysiology2-201006142544/85/Cell-physiology2-45-320.jpg)