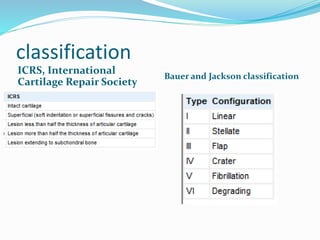
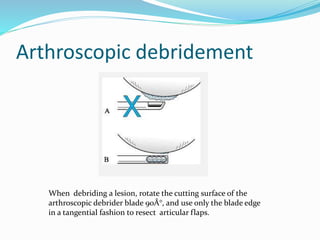
Cartilage injuries most commonly occur in the knee joints and can affect both young and elderly populations through traumatic or degenerative means. Treatment depends on the severity and location of the injury. For partial thickness injuries, arthroscopic debridement can provide short-term relief. For full thickness injuries, options include stimulating intrinsic healing by microfracture, altering joint loads through osteotomy, transferring autologous tissue through mosaicplasty or chondrocyte implantation, or using allografts. Future approaches may involve gene therapy to enhance the repair process.