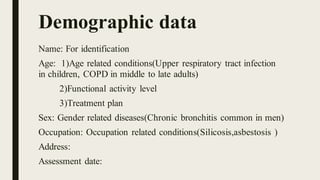
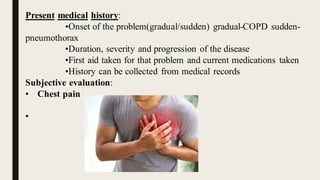
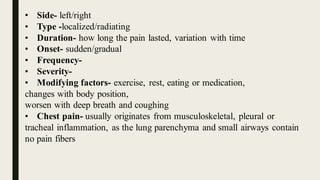
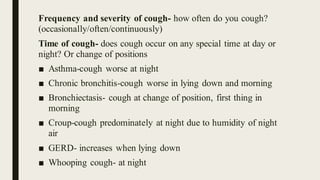
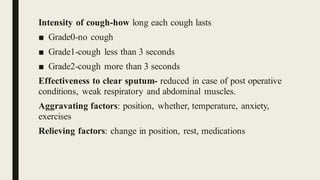
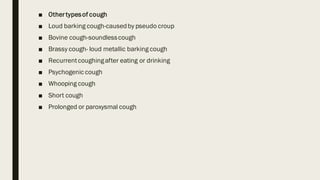
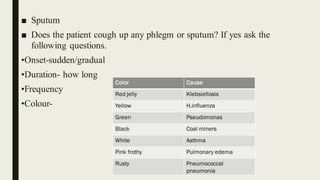
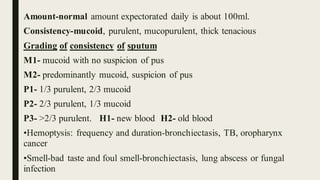
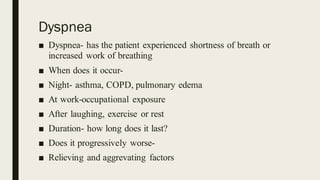
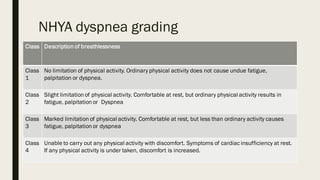
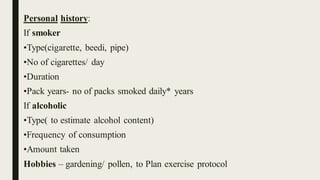
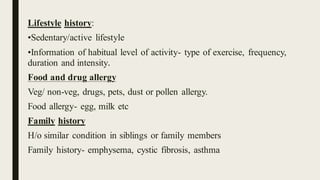
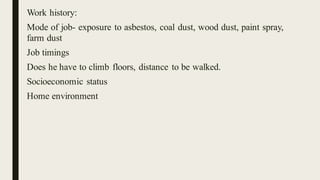
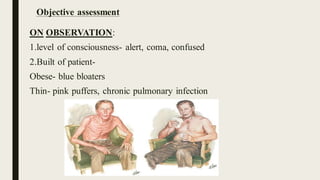
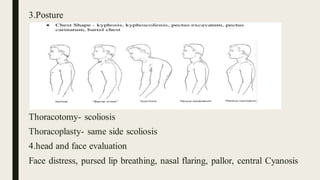
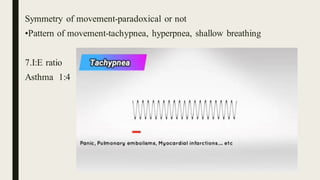
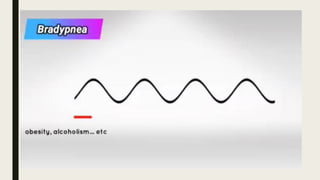
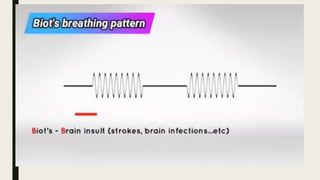
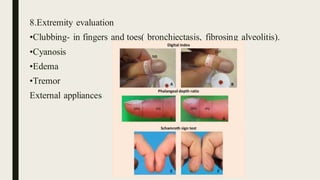
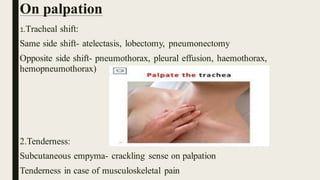
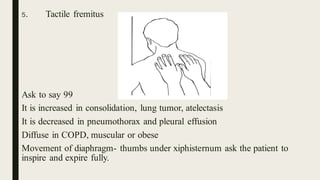
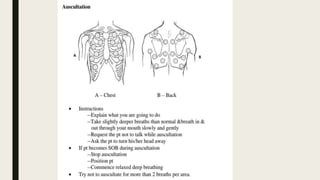
Thomas J. Watson said that asking the right questions is key to finding answers. This document provides guidelines for conducting a respiratory assessment through gathering subjective and objective information. It details questions to ask about symptoms like cough, sputum, dyspnea and wheezing and how to examine vital signs, breathing patterns, chest expansion and auscultated lung sounds. The goal is to collect relevant medical history and evaluate respiratory function and symptoms.