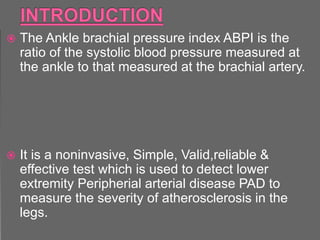
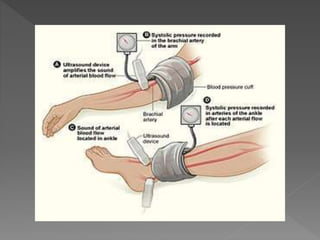
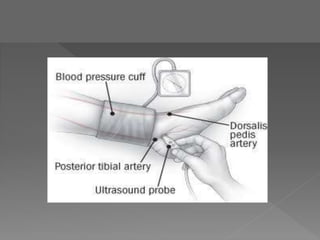
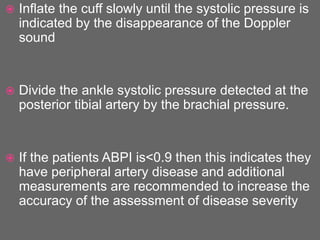
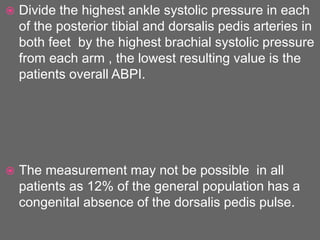
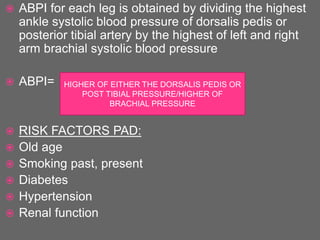
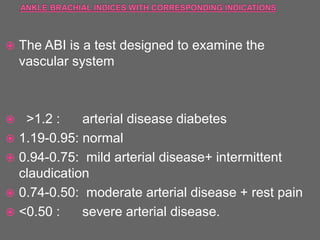
The document outlines the learning objectives and clinical applications of the Ankle Brachial Index (ABI) test, which is a noninvasive method for detecting peripheral arterial disease (PAD) through the comparison of blood pressure measurements at the ankle and arm. It highlights the sensitivity, specificity, and limitations of the ABI, including its inability to determine the exact location of arterial stenosis and risks of false positives in certain conditions. The document also discusses risk factors for PAD and presents clinical signs indicating the severity of arterial insufficiency.