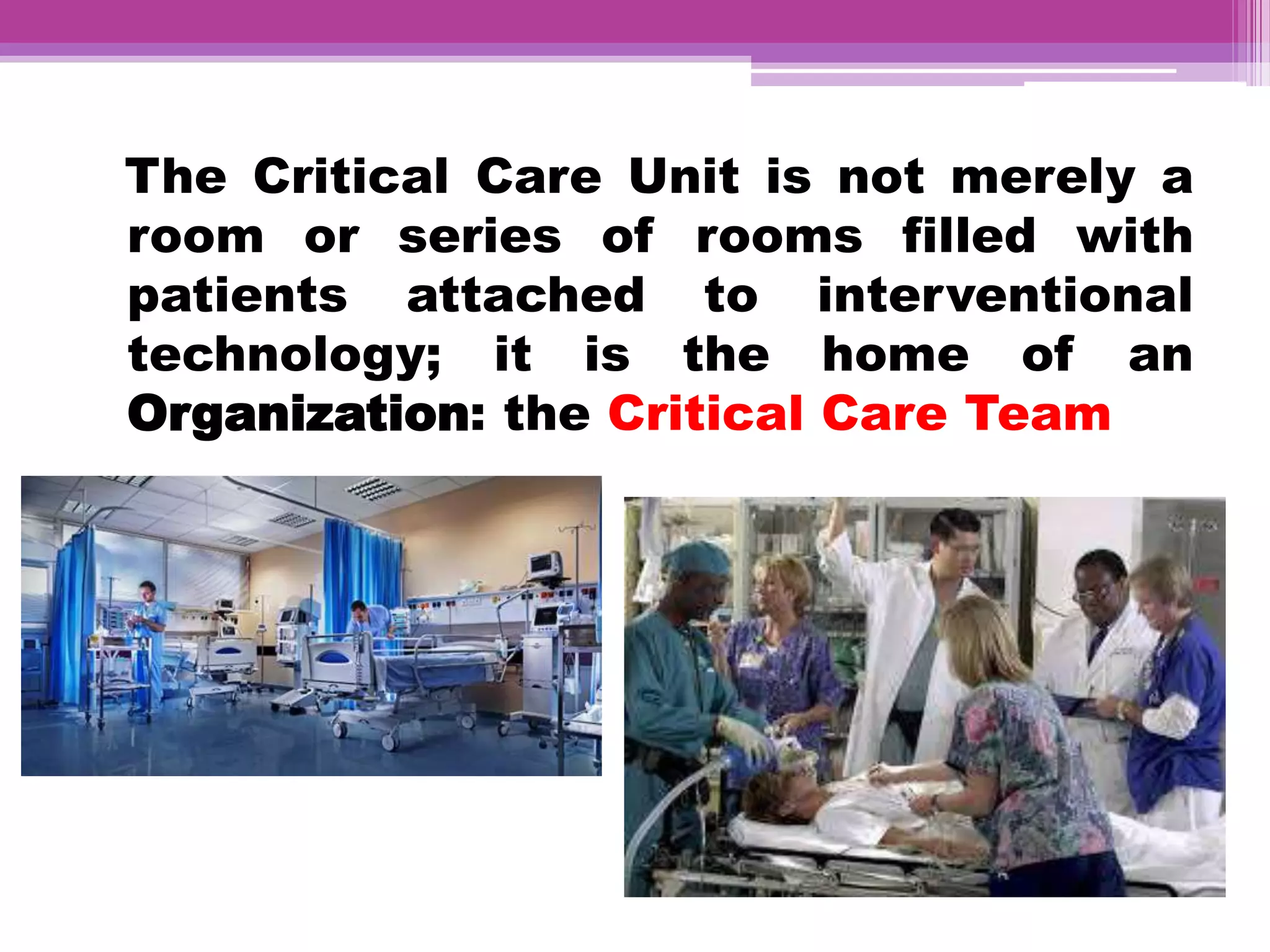
The document discusses critical care nursing and the organization and design of intensive care units (ICUs). It defines critical care nursing and its roles/responsibilities. It describes the evolution of ICUs and different levels of ICUs. It discusses the organization of ICUs including staffing, equipment, patient areas, central nursing station, and other therapeutic and support areas. The principles of critical care nursing are also outlined.