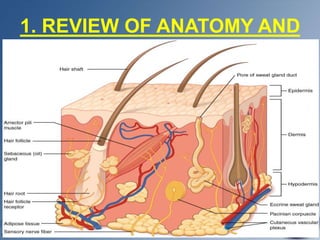
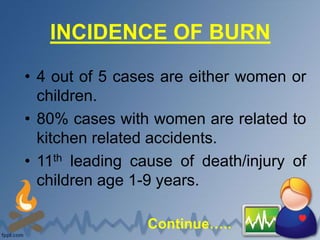
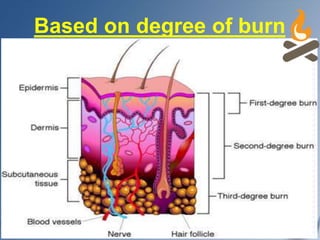
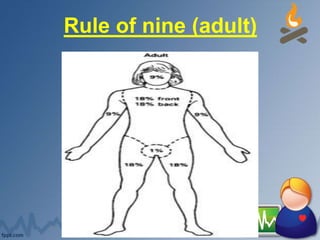
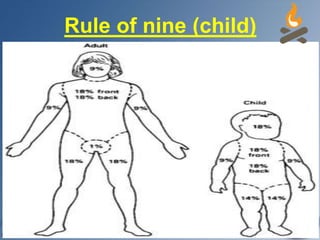
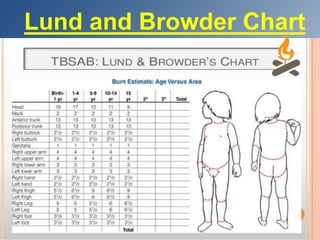
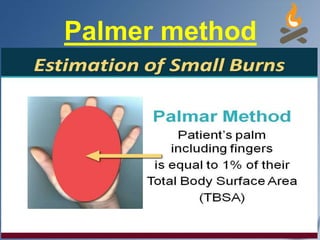
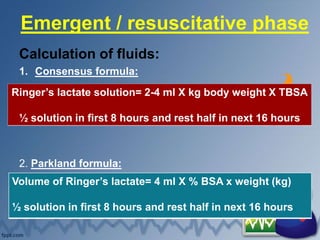
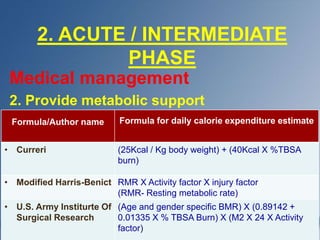
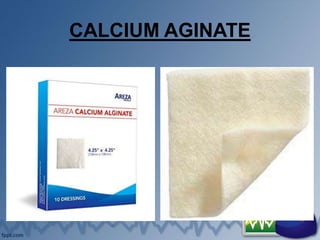
This document provides an overview of burns, including their anatomy, physiology, incidence, causes, classifications, stages of treatment, complications, and nursing management. It begins with definitions of burns and classifications according to depth and extent. It then discusses the pathophysiology and presents the three phases of burn care - emergent/resuscitative, acute/intermediate, and rehabilitation. Nursing priorities and treatments are outlined for each phase, including wound care, pain management, and psychological support. Surgical procedures and potential complications are also reviewed.