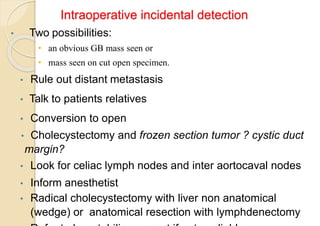
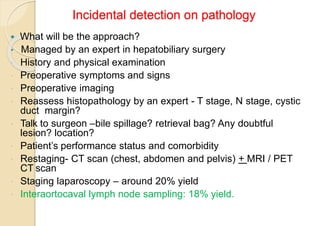
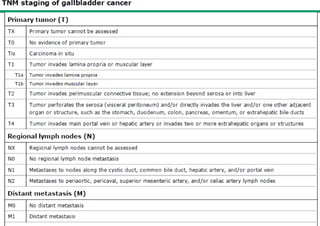
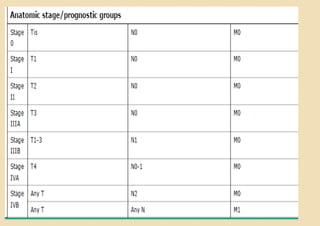
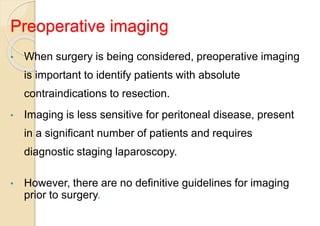
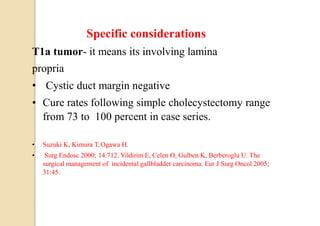
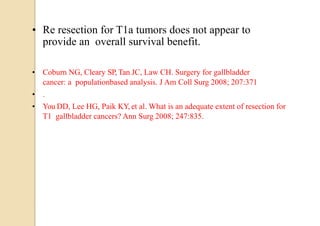
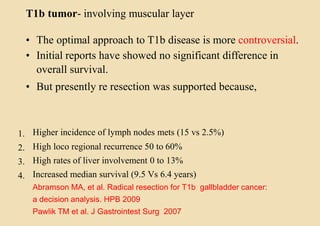
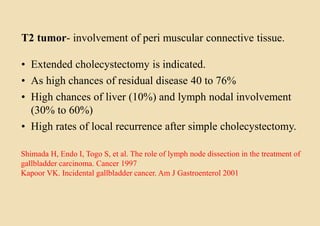
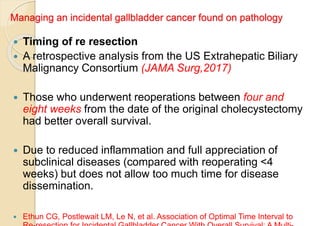
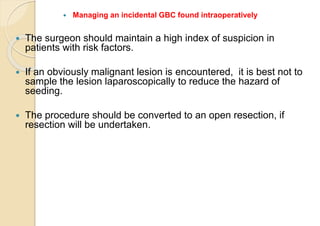
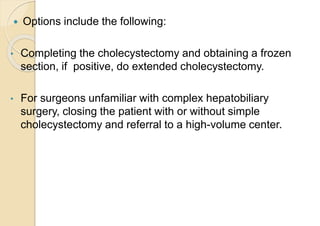
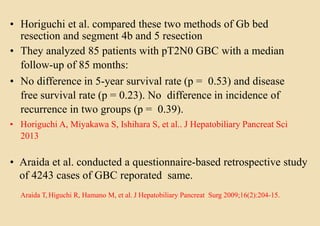
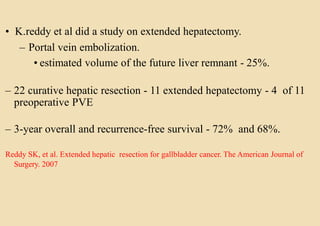
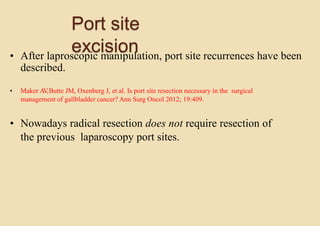
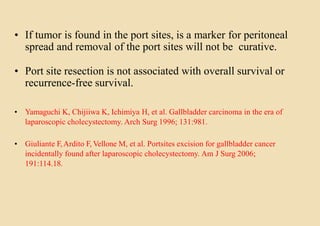
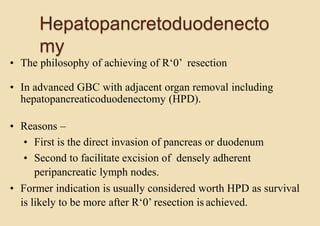
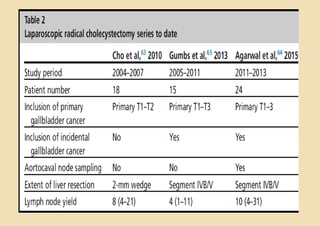
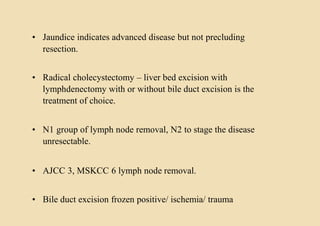
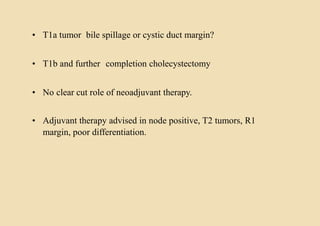
This document discusses the management of gallbladder cancer. It covers diagnosis, staging, and surgical treatment approaches based on tumor stage. For early stage T1a tumors found incidentally after cholecystectomy, simple cholecystectomy may be adequate. For T1b and T2 tumors, radical resection including lymph node dissection is recommended due to higher risk of residual disease and lymph node involvement. For locally advanced T3/T4 or node positive cancers, radical surgery with hepatic resection or multi-organ resection is supported, though morbidity and mortality are high; N2 node involvement carries a poor prognosis. Staging laparoscopy is important to identify unresectable disease not apparent on imaging.