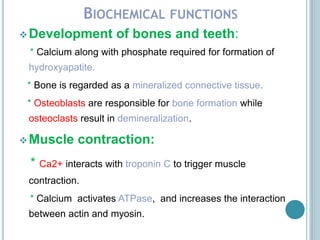
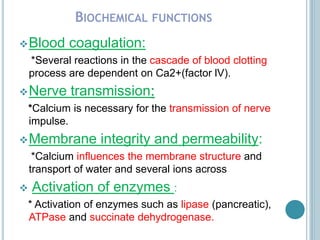
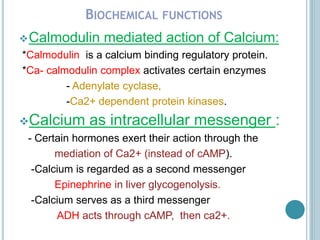
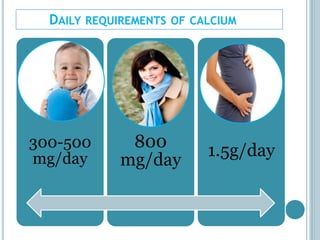
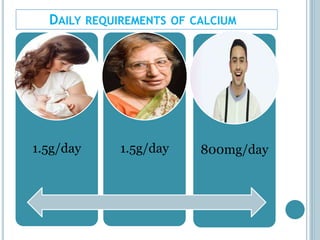
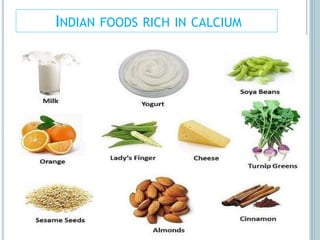
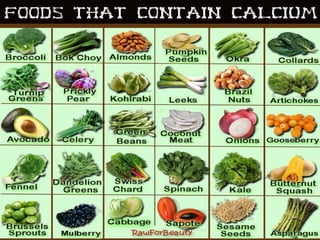
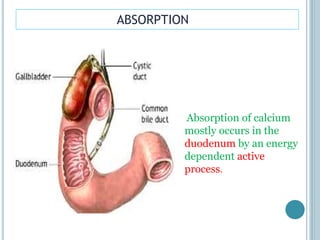
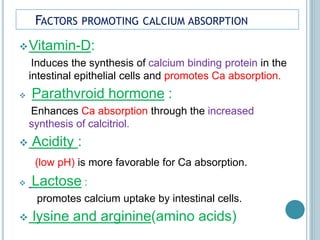
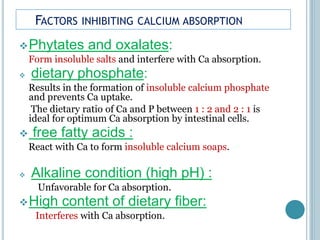
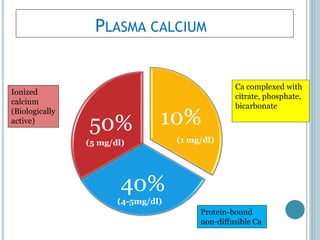
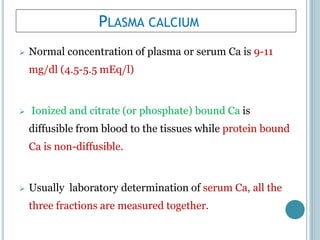
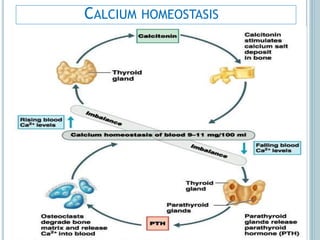
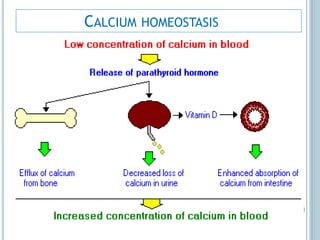
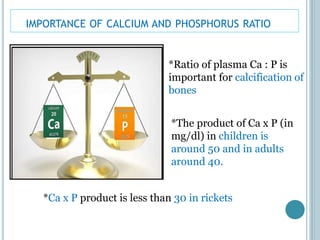
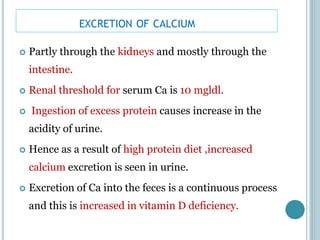
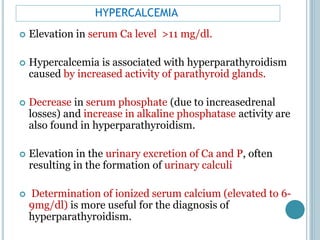
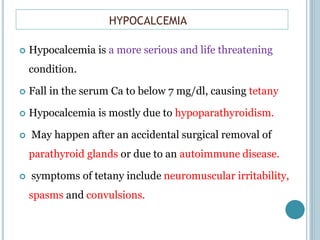
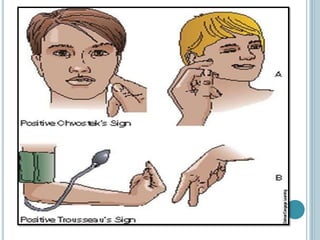
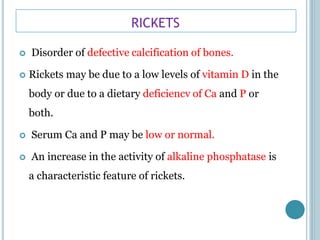
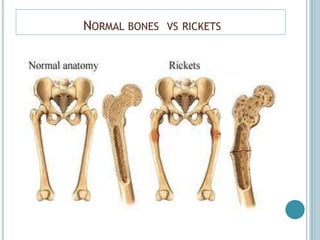
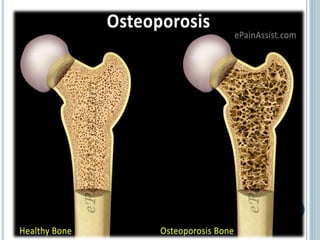
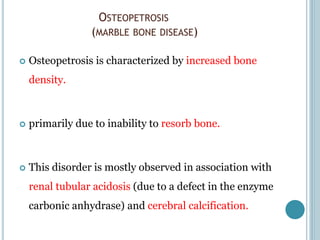
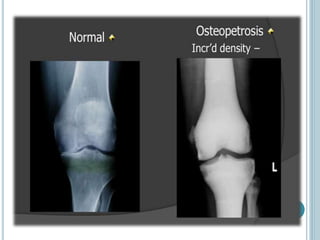
The document discusses calcium's biochemical functions including roles in bone and teeth formation, muscle contraction, blood coagulation, nerve transmission, and enzyme activation. It describes calcium requirements, sources, absorption factors, homeostatic regulation by parathyroid hormone, calcitonin, and vitamin D, and excretion. It also examines diseases like hypercalcemia, hypocalcemia, rickets, osteoporosis, and osteopetrosis.