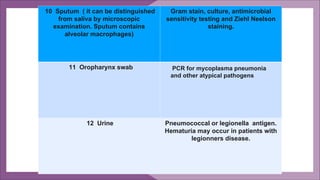
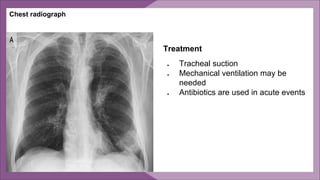
Pneumonia is an inflammation of the lungs that can have multiple causes. It is typically caused by bacterial, viral or fungal infections. Pneumonia can be classified based on location in the lungs, cause, or clinical setting. Common symptoms include cough, fever, chest pain and difficulty breathing. Diagnosis involves physical exam, chest x-ray, blood tests and sputum/fluid cultures. Treatment focuses on antibiotics, oxygen therapy and treatment of complications. Hospital-acquired pneumonia requires broader-spectrum antibiotics due to more drug-resistant organisms. Prevention emphasizes hand hygiene, limiting aspiration and prudent antibiotic use.