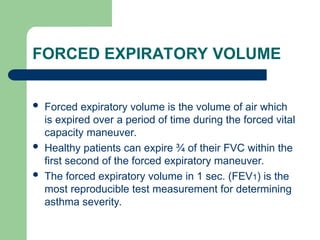
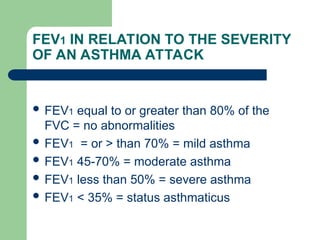
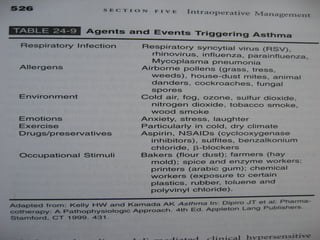
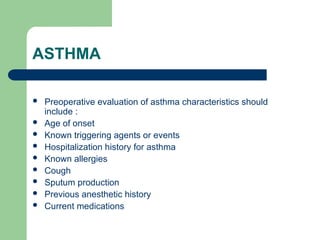
The document discusses asthma as an inflammatory disorder causing airway obstruction and details its prevalence and medical implications, particularly in relation to anesthesia. It outlines classifications of asthma severity based on forced expiratory volume (FEV1) and provides guidelines for preoperative evaluation, drug therapy, and anesthetic management to minimize complications. Key treatment strategies include avoiding certain risk factors, using inhaled bronchodilators, and ensuring smooth anesthetic induction and emergence to prevent bronchospasm.