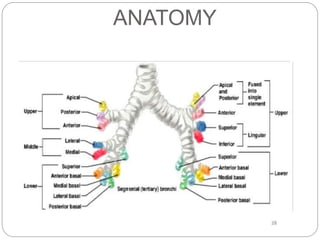
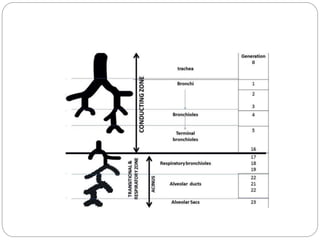
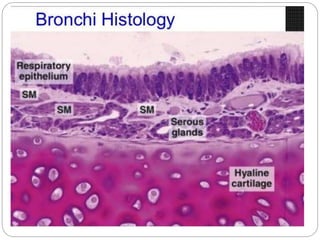
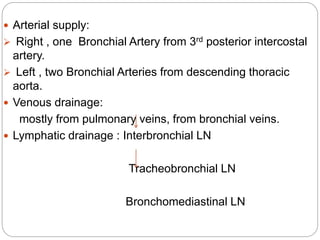
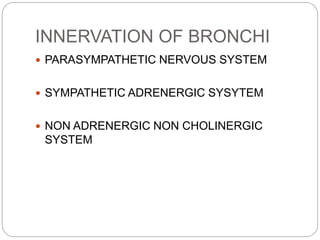
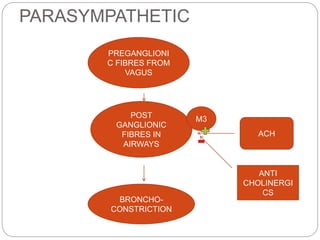
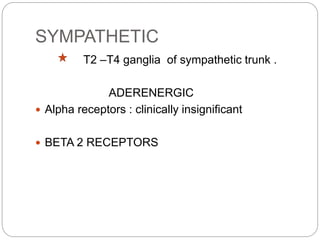
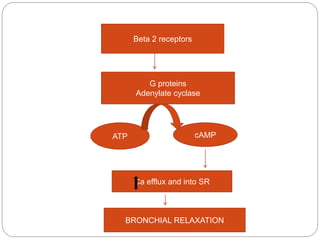
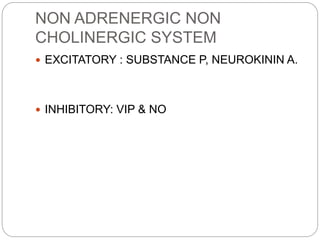
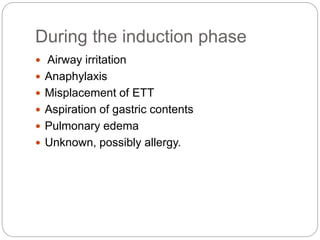
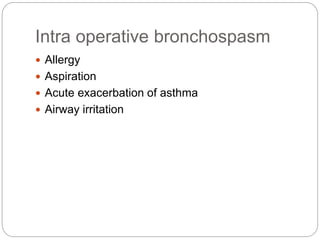
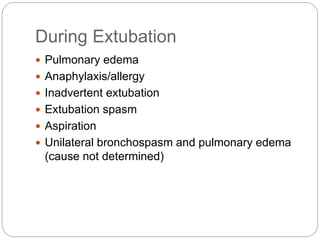
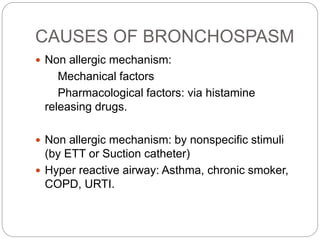
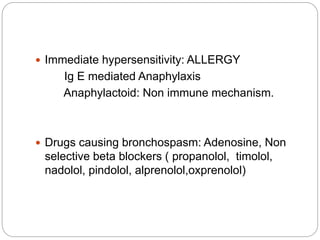
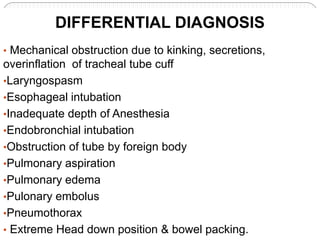
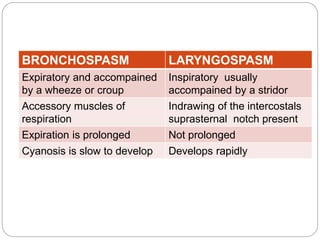
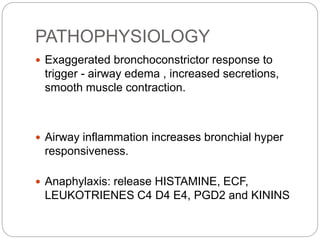
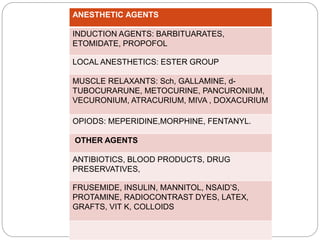
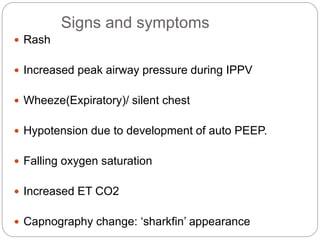
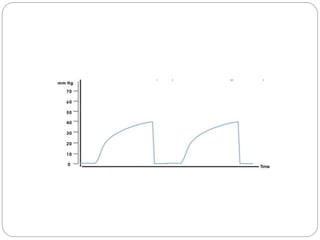
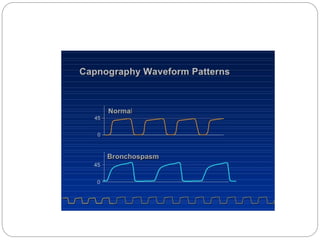
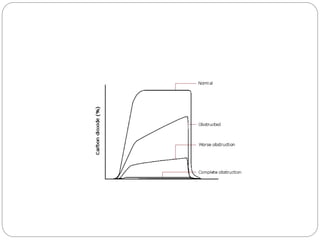
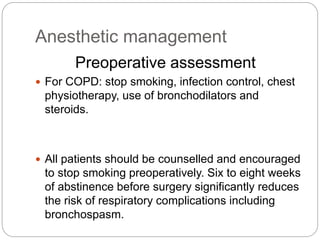
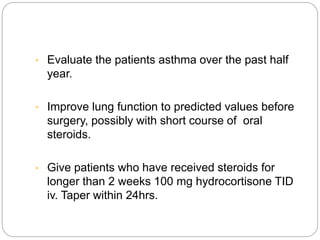
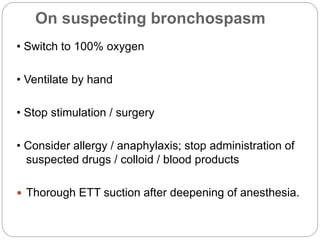
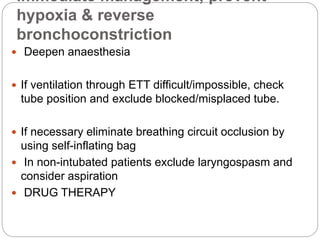
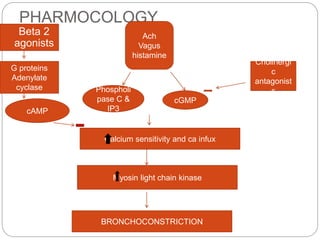
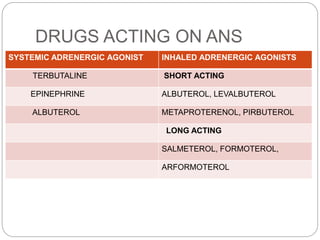
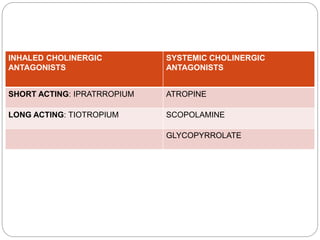
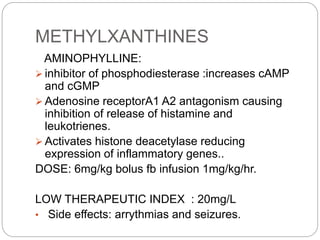
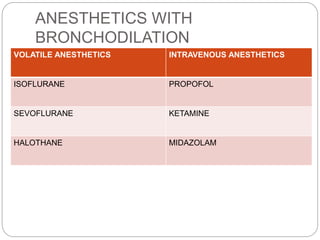
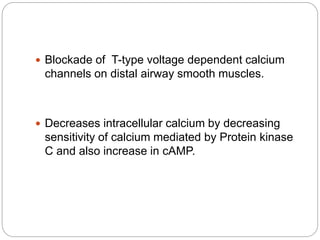
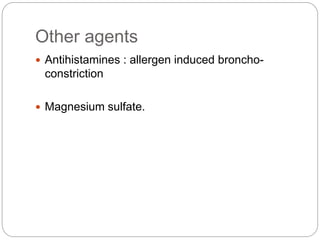
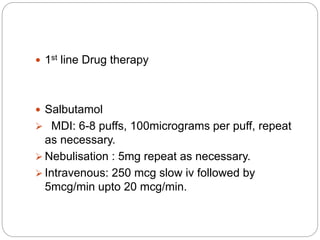
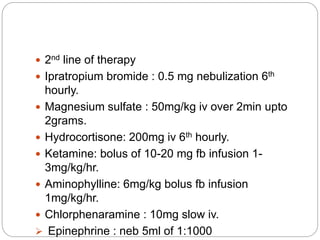
Dr. Imran's document discusses the management of intraoperative bronchospasm. It defines bronchospasm as constriction of the smooth muscles of the bronchi and bronchioles. It then covers the anatomy, innervation, causes, signs and symptoms, diagnosis, pathophysiology, anesthetic agents that can cause it, and treatment of bronchospasm. The treatment involves deepening anesthesia, administering bronchodilators like salbutamol, and other drugs like ipratropium bromide, magnesium sulfate, and hydrocortisone to reverse bronchoconstriction and prevent hypoxia.