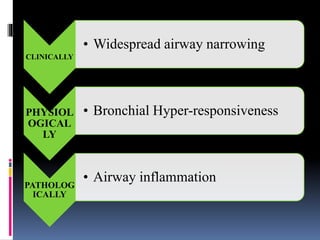
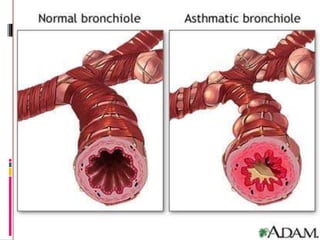
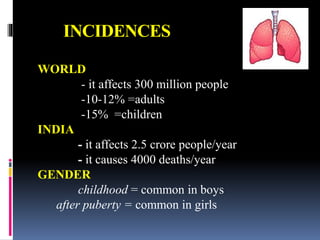
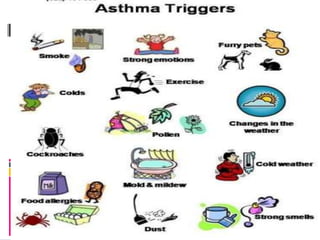
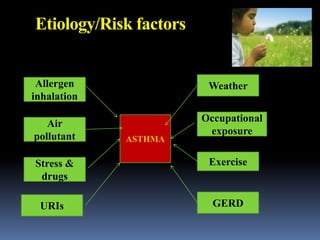
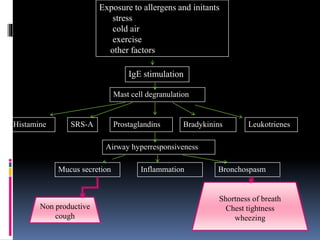
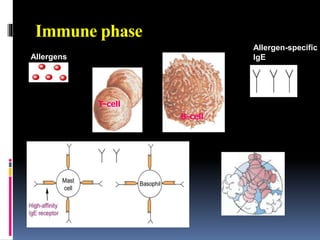
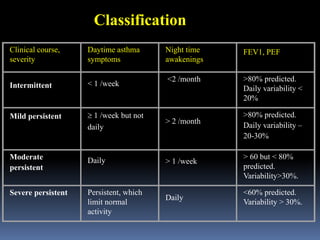
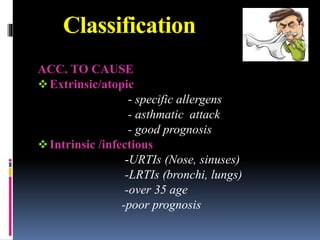
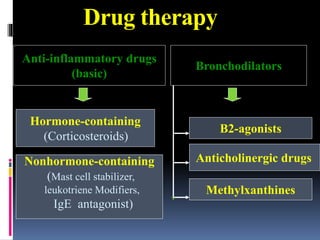
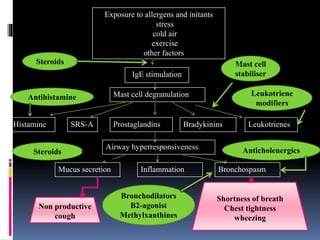
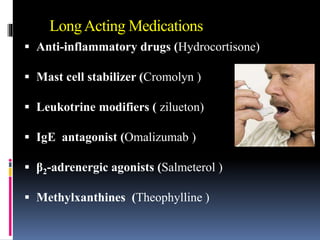
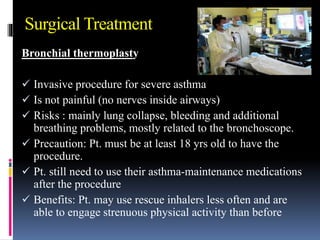
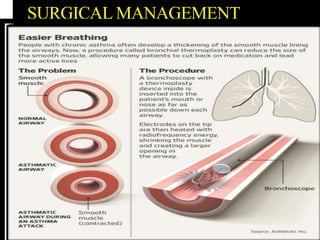
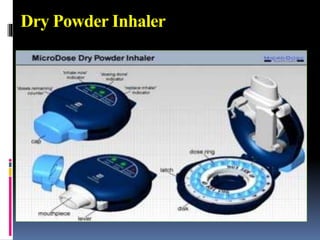
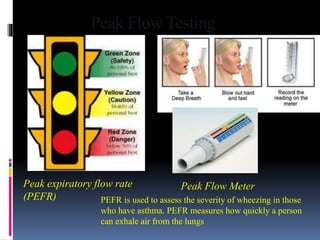
Bronchial asthma is a chronic inflammatory lung disease that causes narrowing of the airways. It is characterized by recurrent episodes of wheezing, breathlessness, chest tightness, and coughing. Risk factors include allergens, air pollution, infections, stress, obesity, and family history. Symptoms are typically worse at night or early morning. Diagnosis involves assessing symptoms and lung function tests. Treatment focuses on preventing symptoms through avoidance of triggers and use of inhaled corticosteroids and bronchodilators. Nursing care emphasizes breathing treatments, monitoring for complications, patient education, and managing exacerbations.