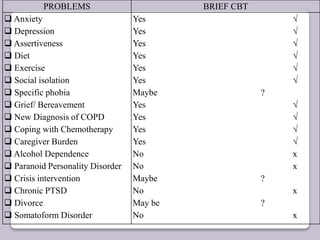
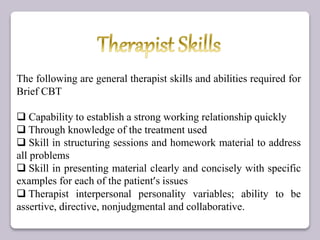
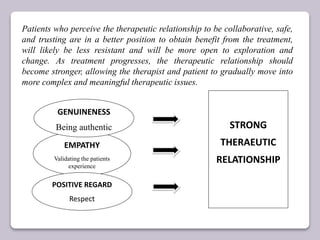
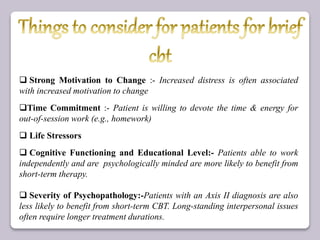
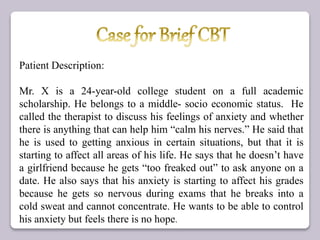
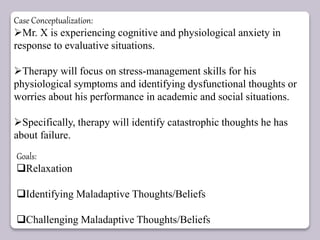
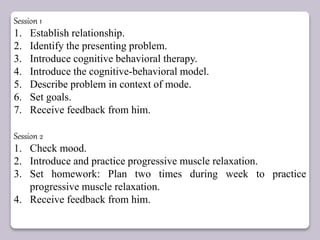
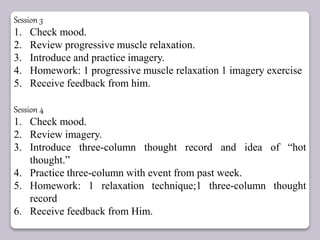
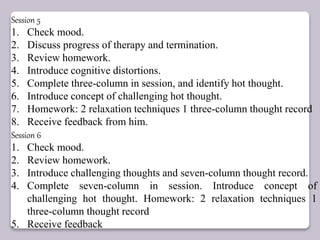
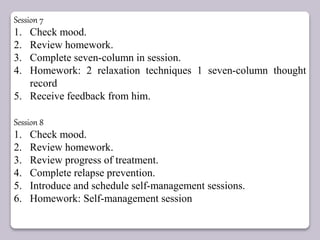
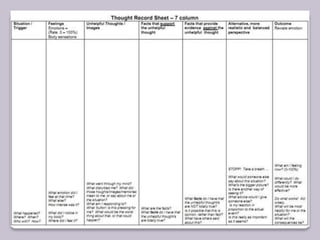
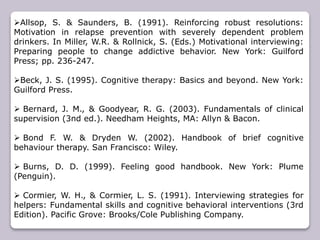
Brief CBT involves compressing traditional CBT into 4-8 sessions by focusing on specific problems. It is effective for issues like anxiety, depression, and social isolation. The document outlines the skills needed by therapists for brief CBT, including establishing rapport, structuring sessions, and presenting material clearly. It then presents a case study of a student with anxiety affecting his grades and relationships, conceptualizing the issues and outlining an 8 session brief CBT treatment plan focusing on relaxation, challenging thoughts, and preventing relapse.