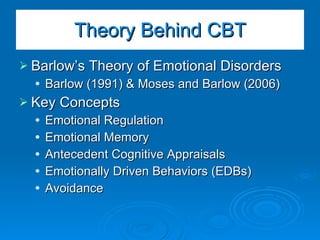
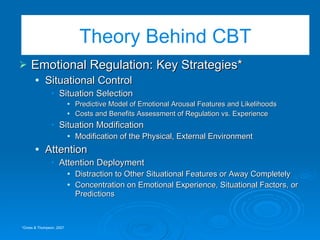
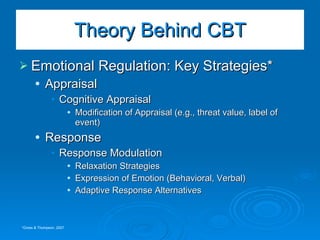
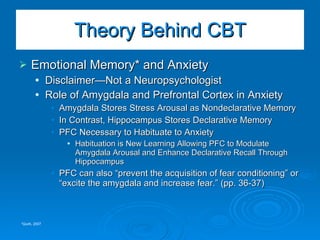
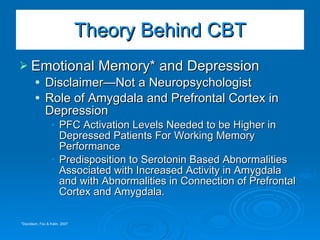
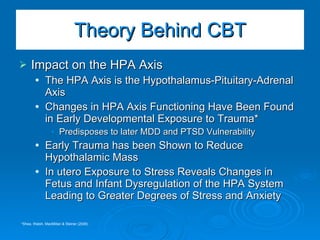
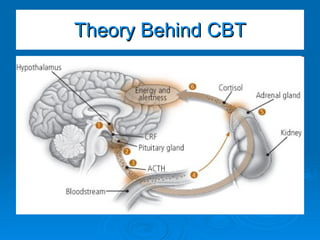
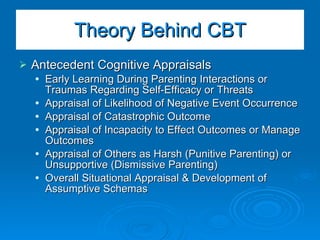
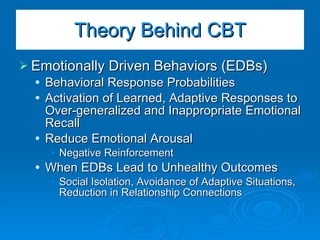
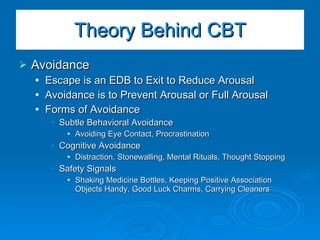
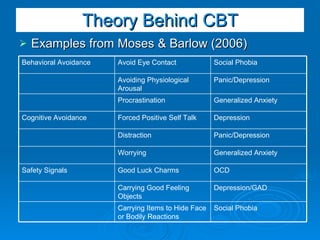
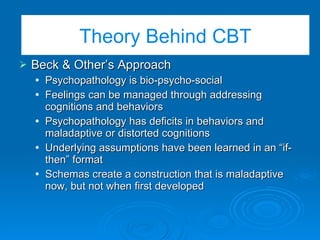
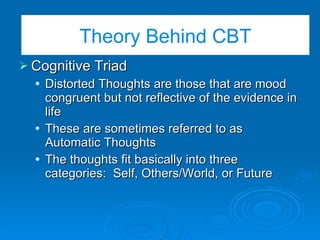
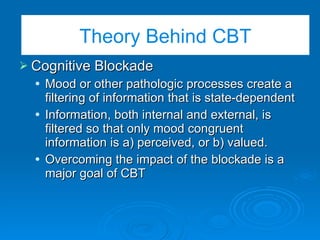
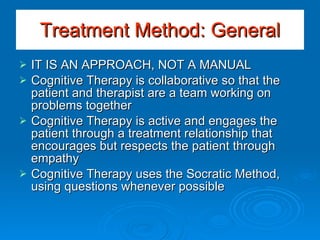
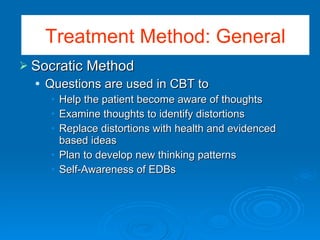
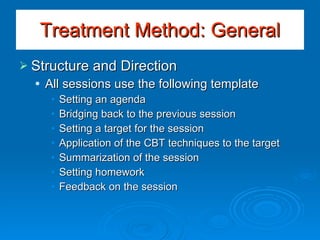
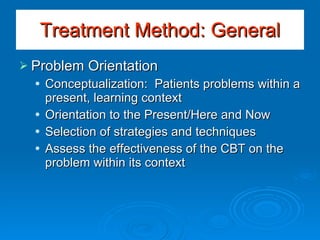
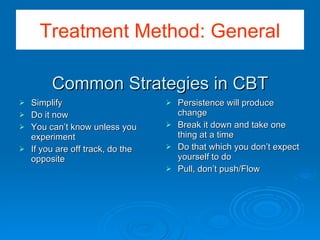
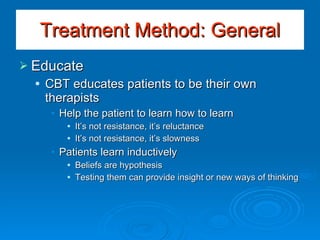
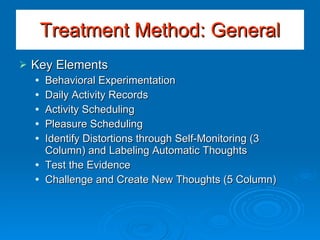
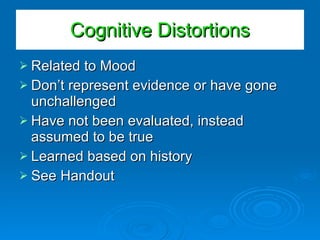
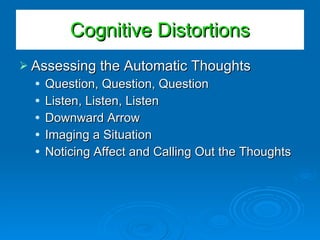
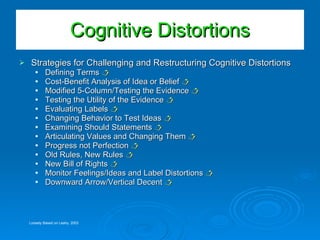
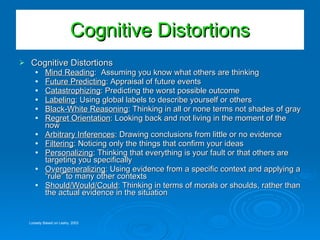
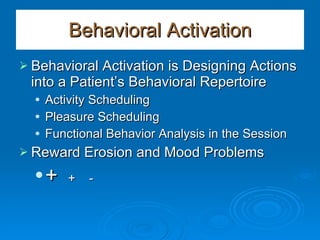
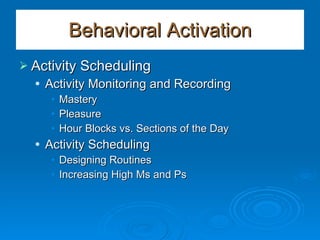
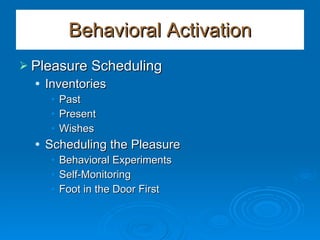
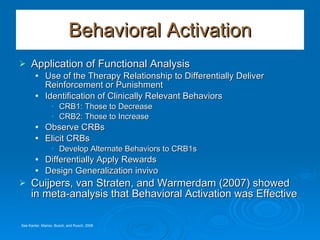
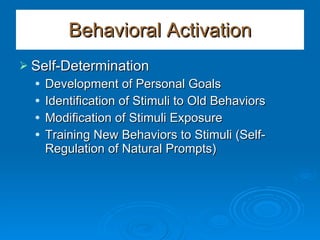
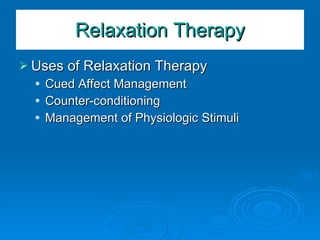
The document provides an overview of cognitive-behavioral therapy (CBT) strategies and techniques. It discusses Barlow's model of emotional disorders and how CBT addresses emotional regulation, cognitive appraisals, emotionally-driven behaviors, and avoidance. The basic CBT model examines psychopathology through a bio-psycho-social lens and addresses maladaptive cognitions and behaviors. Common CBT techniques include identifying cognitive distortions, challenging thoughts through questioning and experimentation, and behavioral activation methods like activity scheduling.