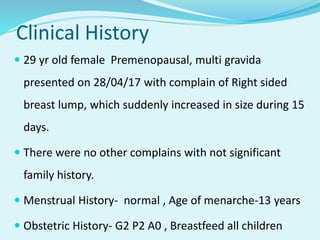
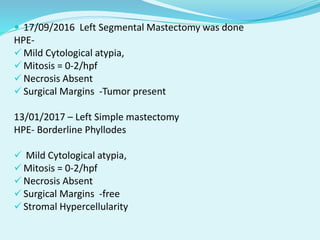
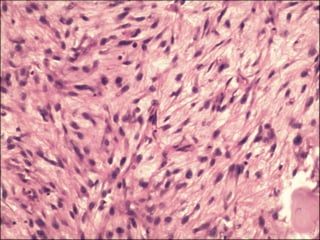
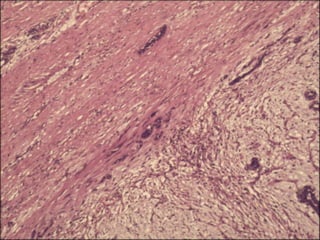
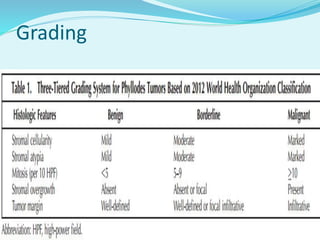
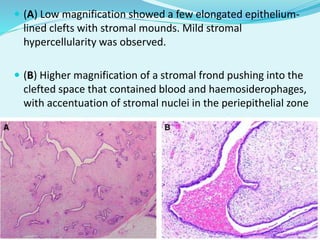
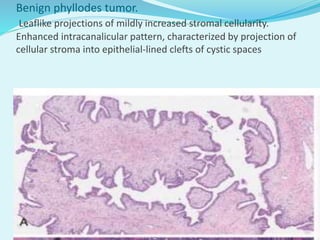
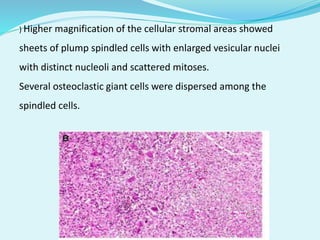
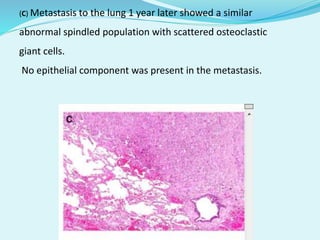
This document discusses a case study of a 29-year-old female patient who presented with a rapidly growing right breast lump. She had a history of multiple surgeries for left breast lumps, with the most recent being a left simple mastectomy in January 2017 that showed a borderline phyllodes tumor. Investigations of the current right breast lump showed features consistent with a phyllodes tumor. She underwent a right simple mastectomy in May 2017, and the pathology again showed a borderline phyllodes tumor. The document then discusses grading of phyllodes tumors, distinguishing between benign and borderline types, and definitions used in grading.