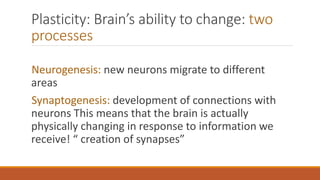
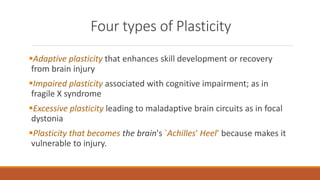
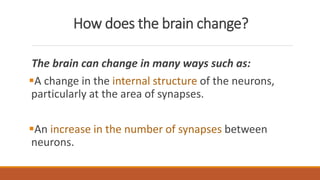
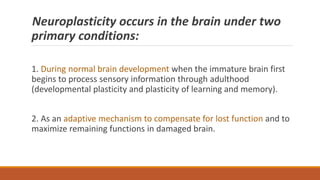
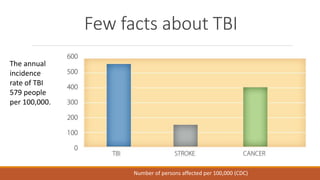
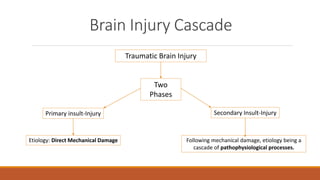
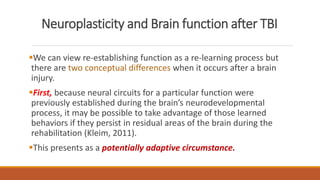
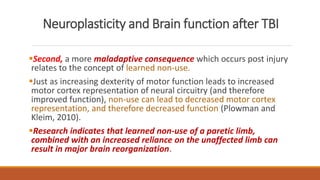
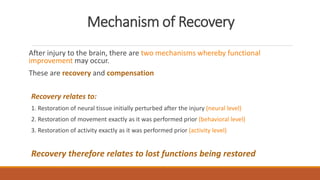
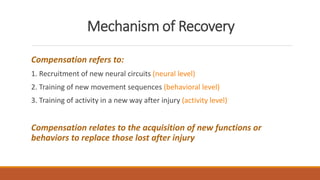
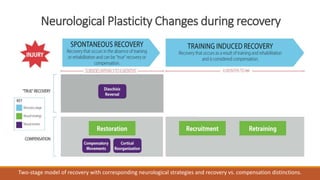
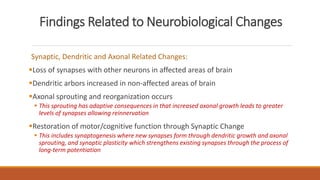
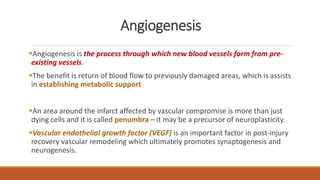
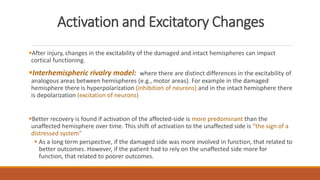
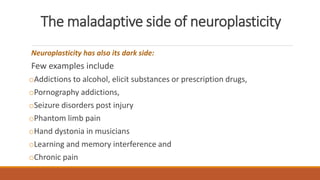
The document discusses brain plasticity, emphasizing its ability to adapt and reorganize in response to challenges, particularly after traumatic brain injury (TBI). It explains the mechanisms of recovery and compensation through neuroplasticity, detailing both spontaneous and training-induced recovery stages. Various factors affecting recovery, including neurogenesis, synaptogenesis, and the rules governing neural adaptation, are highlighted, alongside the darker side of neuroplasticity that can lead to maladaptive conditions.