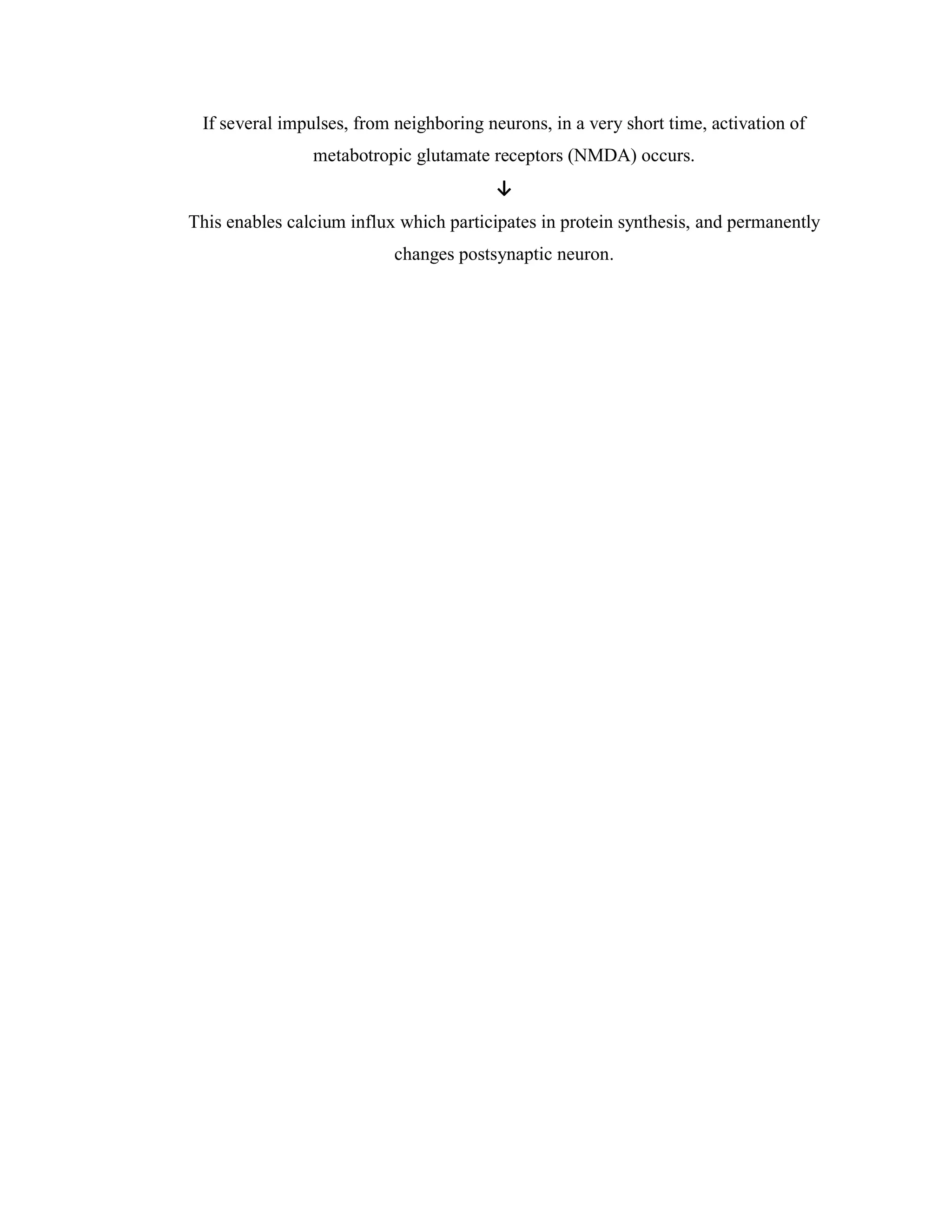
Neuroplasticity refers to the brain's ability to change and reorganize itself in response to experience. The brain forms new connections and pathways when we learn new skills or have new experiences. Neuroplasticity allows the brain to compensate for injury and disease and is responsible for development throughout childhood. Promising therapies that may enhance neuroplasticity include brain stimulation, cognitive training, and certain drugs. Assessing neuroplasticity in humans through biomarkers can help predict treatment response and monitor recovery. Harnessing neuroplasticity is key for rehabilitation from brain injuries and disorders.