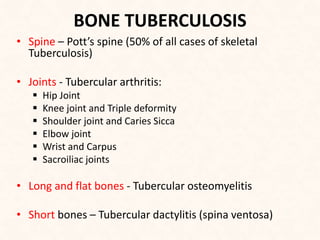
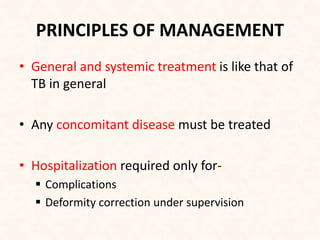
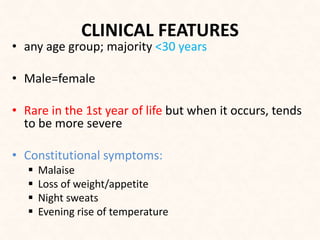
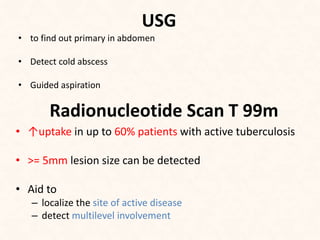
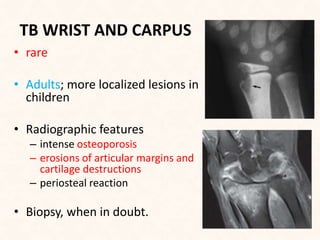
This document discusses bone and joint tuberculosis, providing details on locations, clinical features, investigations, imaging, management, and follow up. It notes that spine and hip tuberculosis are most common, and describes characteristics of tuberculosis in various bones and joints. Imaging modalities like MRI, CT, X-ray, and PET CT are outlined. Surgical indications and conservative treatment including drug therapy are summarized.