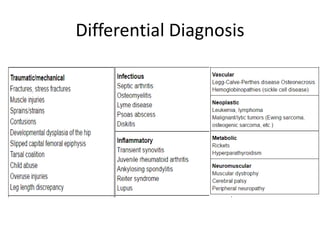
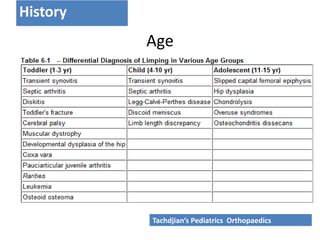
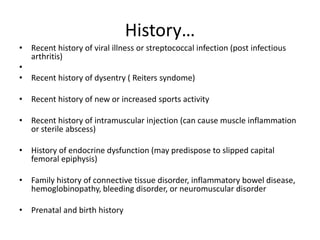
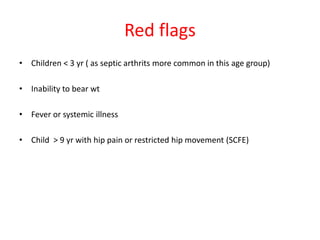
This document provides guidance on evaluating a limping child. It begins with an introduction stating that limping is a common complaint in pediatrics that can be caused by benign or serious conditions. The document then covers pathophysiology, differential diagnosis, history taking, physical exam findings for normal and pathological gaits, investigations including imaging and labs, and key takeaways. The physical exam section describes assessment of gait, standing, supine, and prone positions as well as specific tests. Red flags include age under 3, inability to bear weight, fever or systemic illness. The conclusion emphasizes taking an acute limp seriously and considering age and trauma history in evaluations.

![INTRODUCTION
• An uneven, jerky, or laborious gait, usually caused by pain, weakness, or
deformity.
• It is a common complaint in childhood, accounting for 4 per 1000 visits in
pediatric emergency department. [ Uptodate 2016]
• Limp can be caused by both benign and life-threatening conditions; the
management varies from reassurance to major surgery depending upon
the cause.
INTRODUCTION](https://image.slidesharecdn.com/anapproachtolimpingchild-160706130538/85/An-approach-to-limping-child-2-320.jpg)