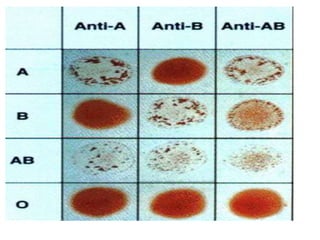
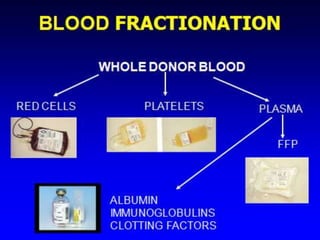
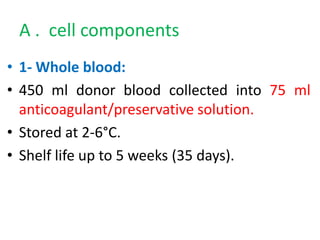
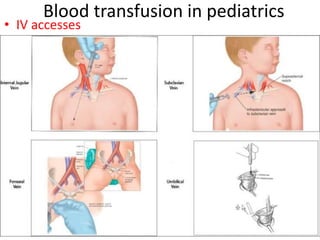
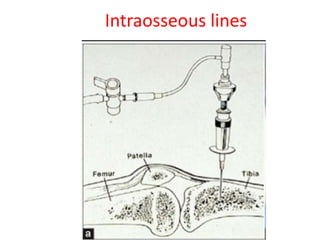
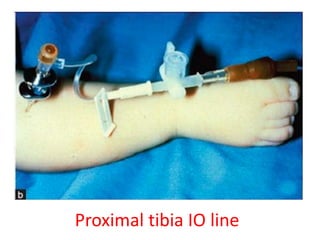
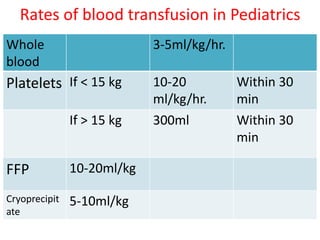
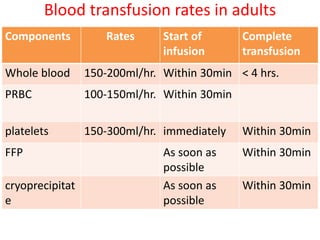
This document defines blood transfusion and its components. It discusses donor selection criteria, blood grouping and cross matching procedures. The main types of blood components are red cell components, platelet concentrate, and plasma. Red cell components include whole blood and packed red cells. Platelet concentrate and fresh frozen plasma contain platelets and coagulation factors, respectively. The document also covers blood transfusion rates for different age groups, as well as potential complications such as allergic reactions, infections, and issues that can arise from massive transfusions.