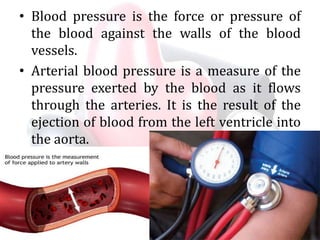
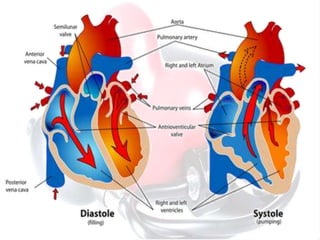
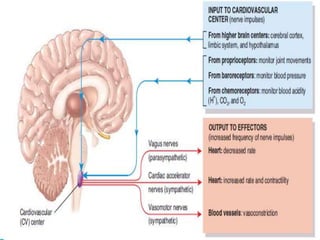
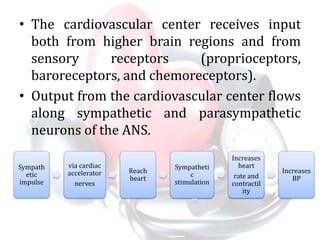
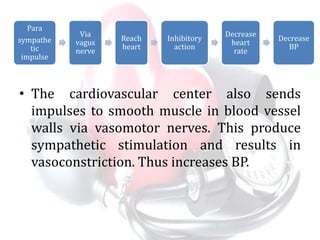
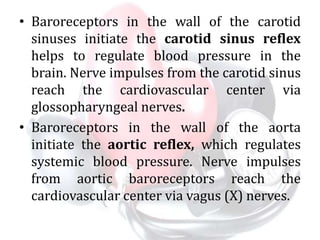
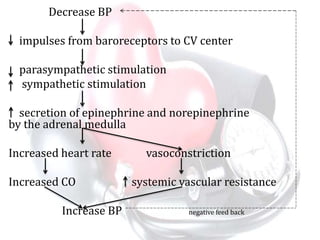
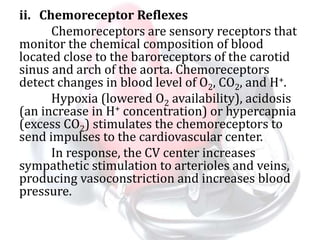
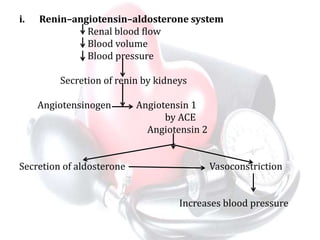
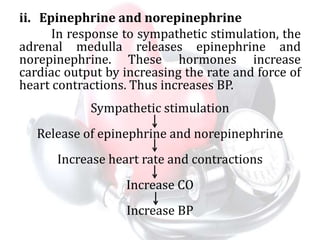
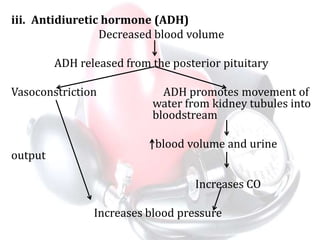
Blood pressure is the force exerted by blood on the walls of arteries. It is measured as systolic over diastolic pressure in mmHg. Systolic pressure occurs when the heart contracts and diastolic when it relaxes. Blood pressure is regulated by the cardiovascular center in the brain through neural mechanisms like baroreceptor and chemoreceptor reflexes and hormonal factors like renin-angiotensin-aldosterone system and epinephrine. Local auto-regulation and factors like age, exercise and stress also affect blood pressure.