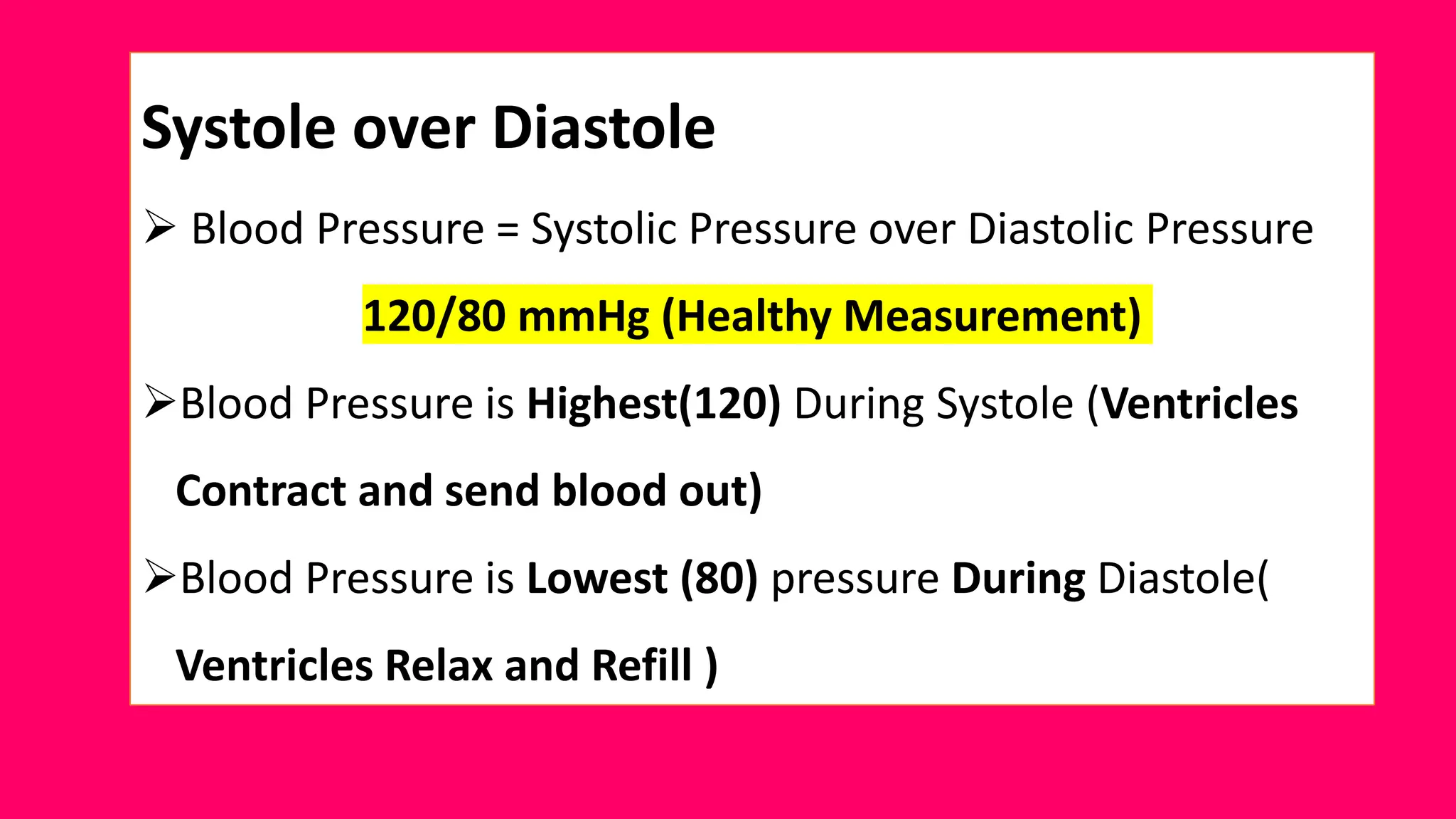
The document provides a comprehensive overview of blood pressure, detailing its definition, measurement, and factors influencing it, such as age, race, diet, and lifestyle. It explains the short-term and long-term regulation of blood pressure through neural and chemical mechanisms, including the renin-angiotensin-aldosterone system (RAAS). Additionally, the document highlights various treatments for hypertension, including ACE inhibitors and diuretics, along with the inflammatory responses associated with the classical RAAS pathway.