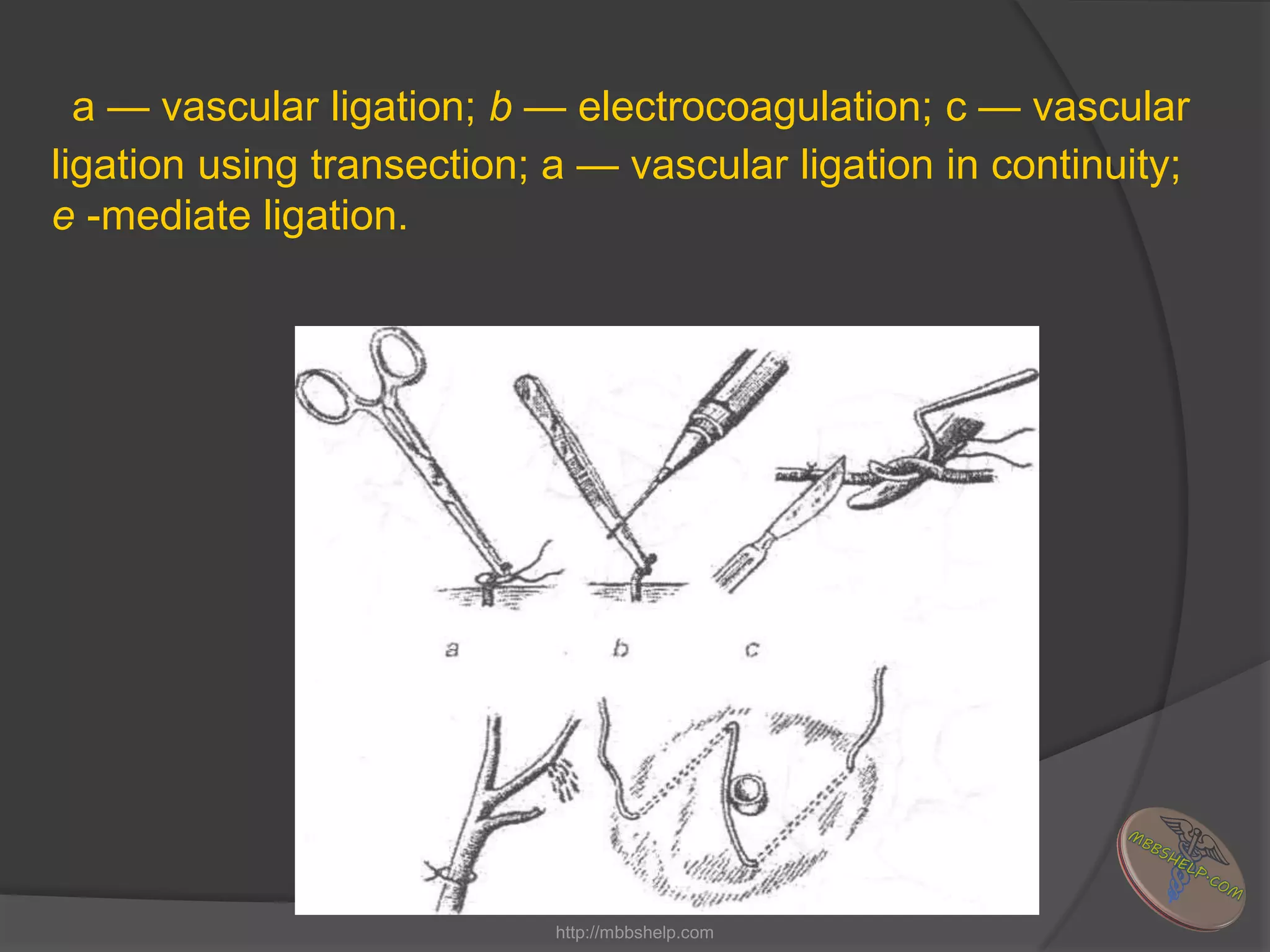
This document discusses bleeding and hemorrhage, describing the different types and causes of bleeding. It defines external bleeding as blood oozing outside the body and internal bleeding as blood accumulating in an enclosed space inside the body. Various methods are presented for controlling bleeding, including both temporary methods like applying a tourniquet or digital compression, as well as definitive methods like ligating blood vessels, vascular sutures, electrocoagulation, and topical hemostatic agents. Laboratory tests for diagnosing and monitoring bleeding are also outlined.