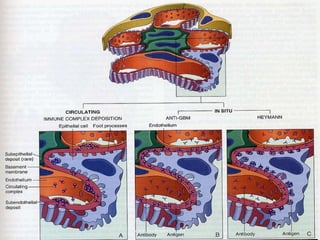
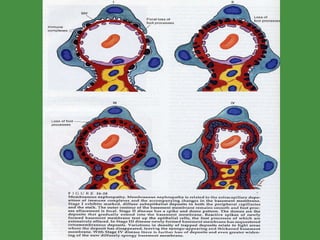
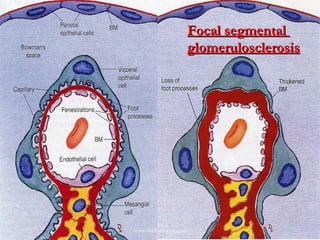
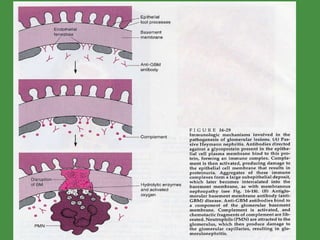
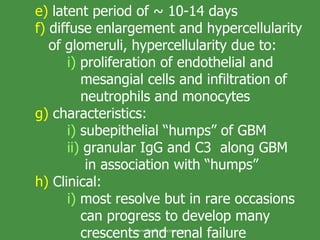
This document summarizes renal pathology and glomerular diseases. It discusses how diseases can affect the glomeruli, tubules, interstitium and vasculature. The glomeruli are described as a network of capillaries lined by endothelial cells, the glomerular basement membrane, and podocytes. Immunological and toxic mechanisms can cause glomerular injury. Membranous glomerulopathy is described as the most common cause of nephrotic syndrome in adults, characterized by thickening of the glomerular capillary wall.


























































































































![Higher risk in smokers and occupational exposure to cadmium 30 fold increase in susceptibility in patients with polycystic disease Classification: a) clear cell Cancer i) most common (70-80% renal ca) b) most are sporadic c) familial links (von Hippel-Lindau [VHL]) i) autosomal dominant disease ii) predispose to a variety of CA – hemangioblastoma of cerebellum and retina www.freelivedoctor.com](https://image.slidesharecdn.com/renalpathology-100417025938-phpapp01/85/Renal-pathology-135-320.jpg)











































































































































![Higher risk in smokers (2:1) and occupational exposure to cadmium, hypertension and acute renal failure and acquired cystic disease. 30 fold increase in susceptibility in patients with polycystic disease Classification: 1. clear cell Cancer i) most common (~ 85 % renal ca) a) most are sporadic (~ 95%), nonpapillary b) familial links (von Hippel-Lindau [VHL]) i) autosomal dominant disease ii) predispose to a variety of CA – hemangioblastoma of cerebellum and retina www.freelivedoctor.com](https://image.slidesharecdn.com/renalpathology-100417025938-phpapp01/85/Renal-pathology-285-320.jpg)








