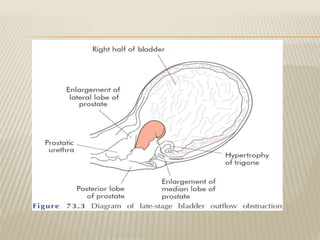
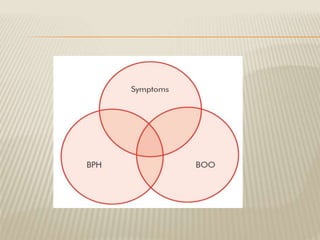
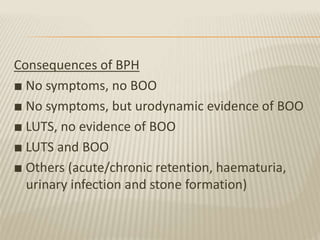
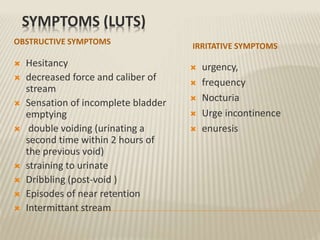
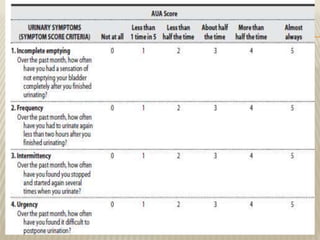
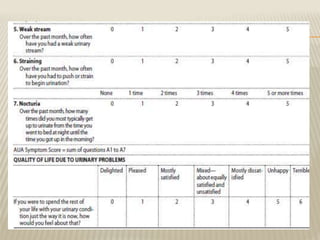
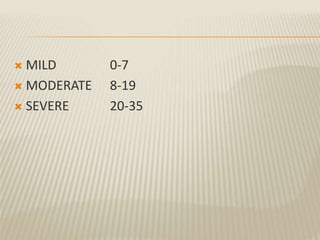
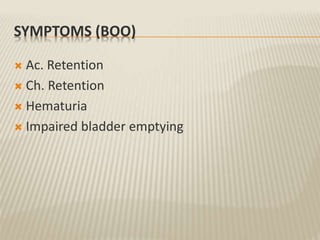
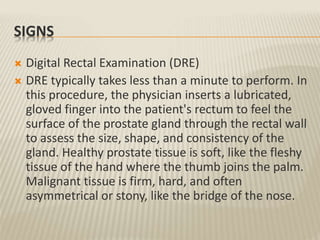
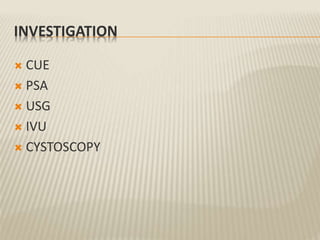
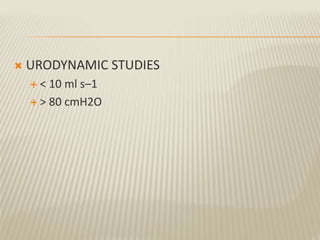
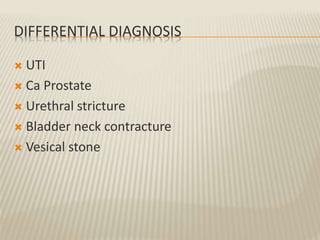
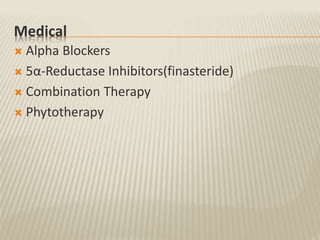
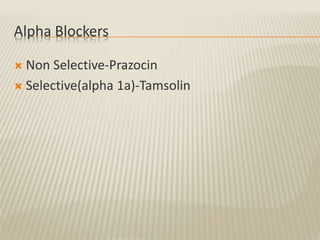
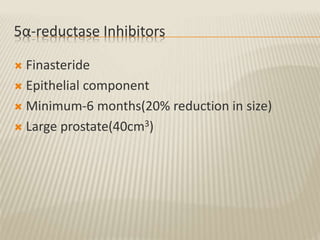
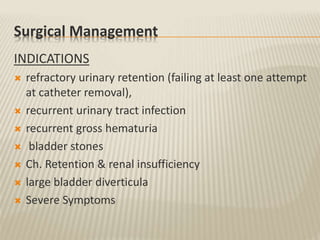
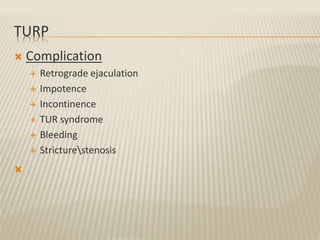
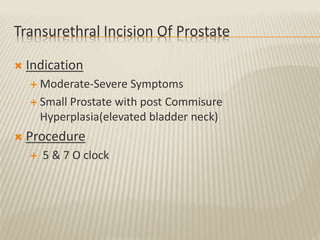
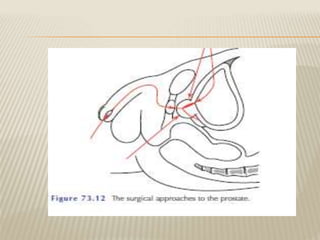
This document discusses benign prostatic hyperplasia (BPH). It notes that BPH is the most prevalent benign tumor in men over 50 years old, with over 90% of men having it by age 80. Symptoms include problems with urination like hesitancy, weak stream, and incomplete emptying. Diagnosis involves digital rectal exam, prostate-specific antigen level, and urodynamic tests. Treatment includes watchful waiting, medications like alpha blockers and 5-alpha reductase inhibitors, and surgeries like transurethral resection of the prostate. Newer minimally invasive options for surgically treating BPH include lasers, electrovaporization, and high-intensity focused ultrasound.