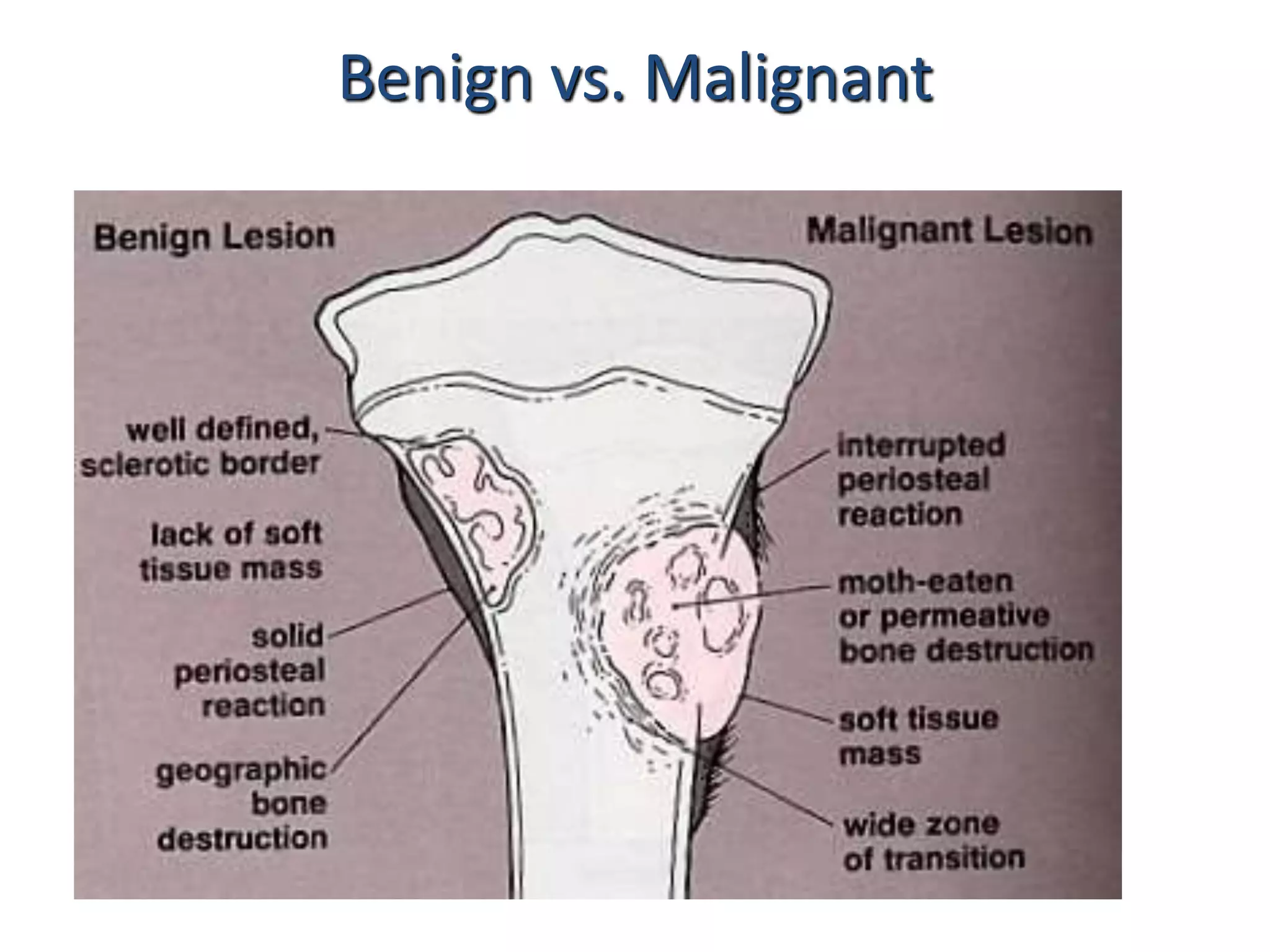
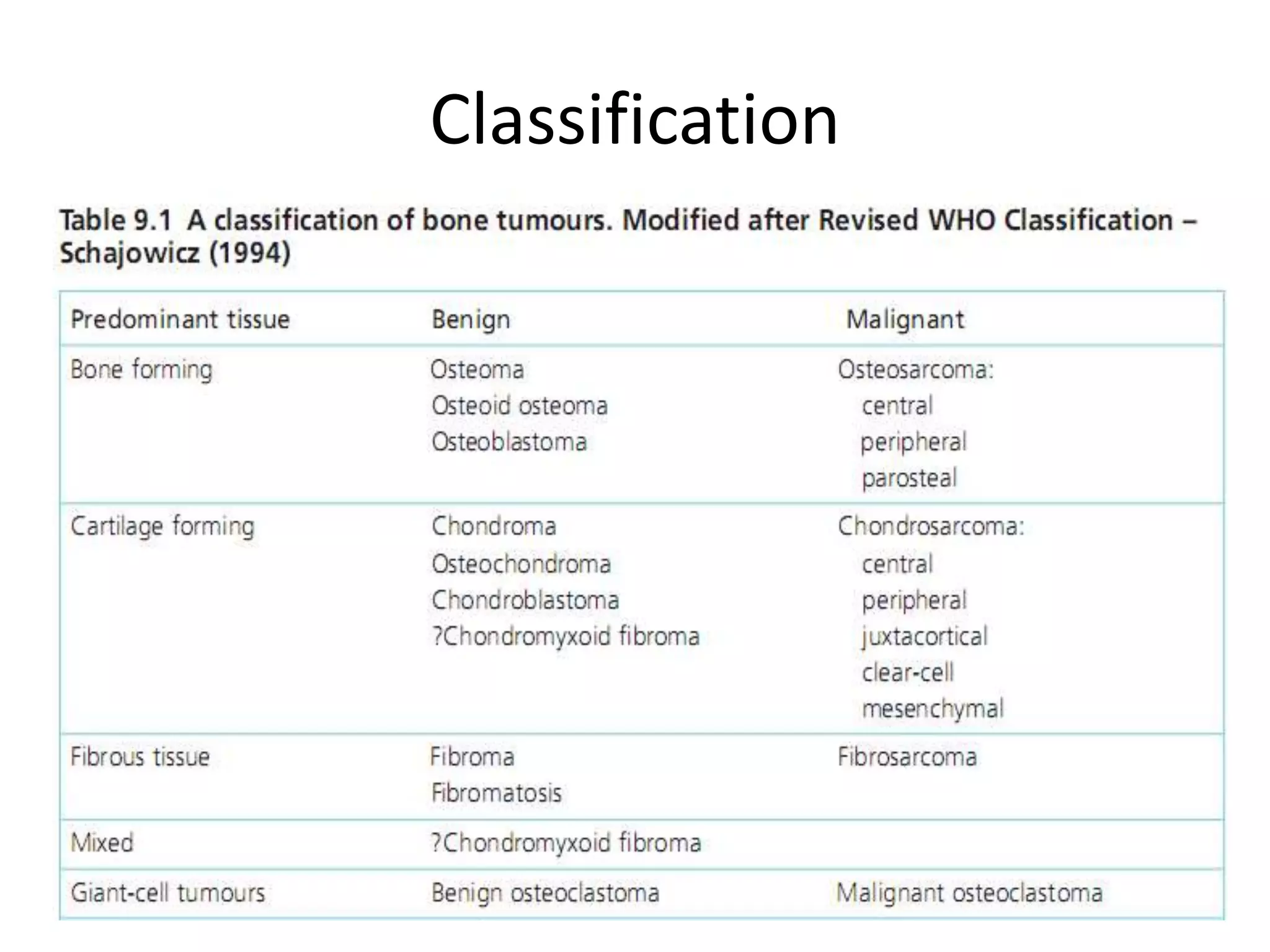
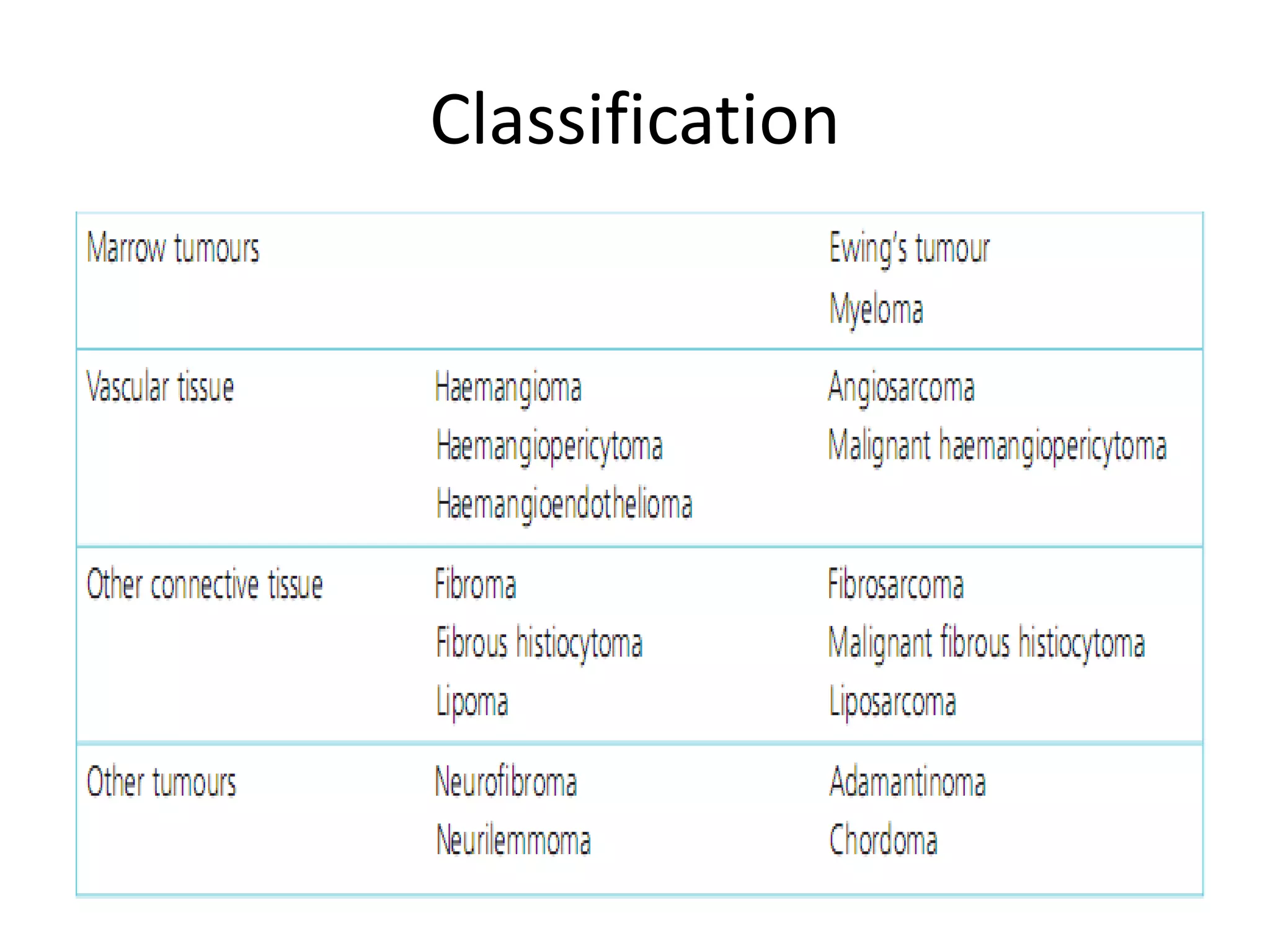
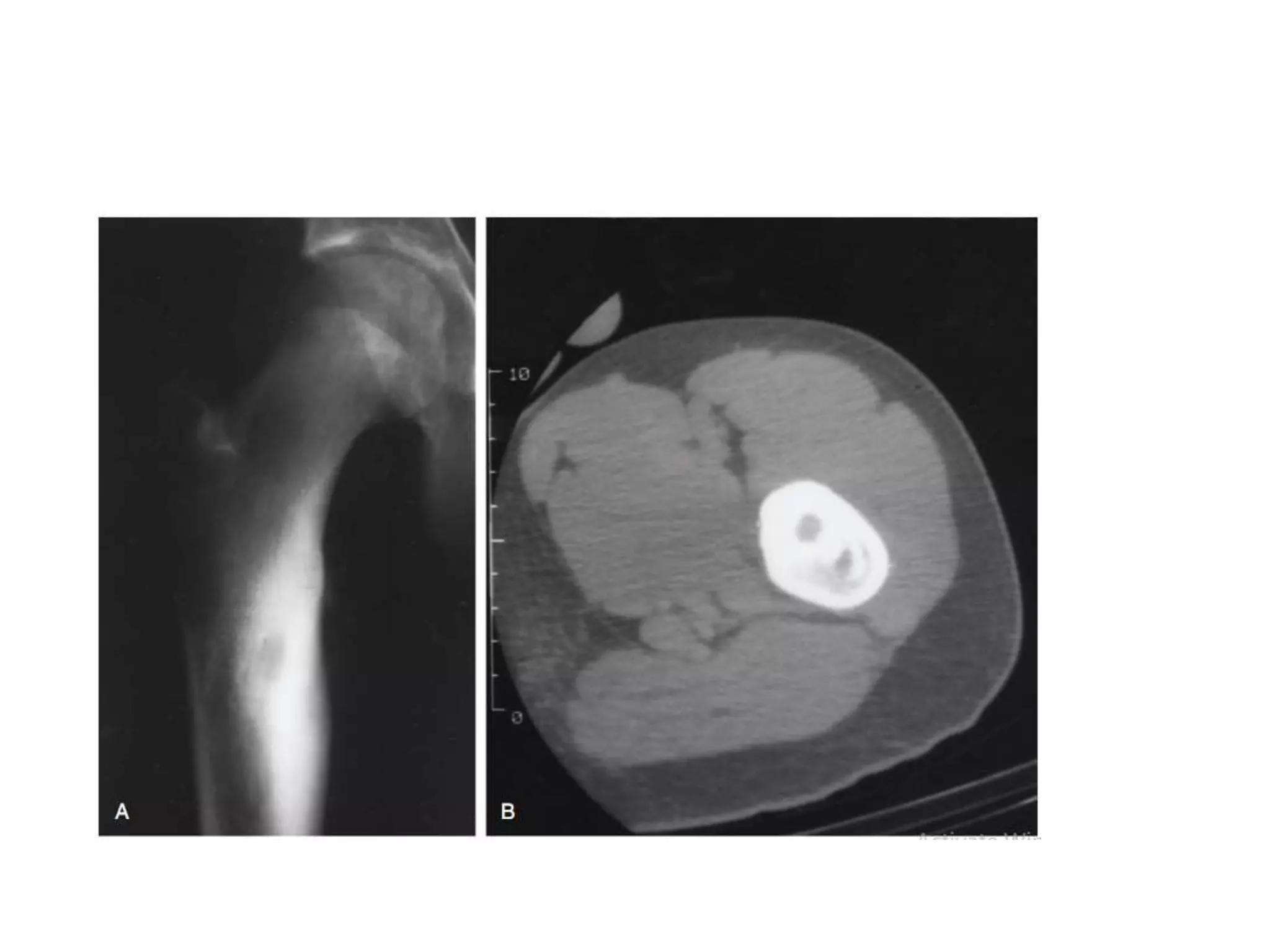
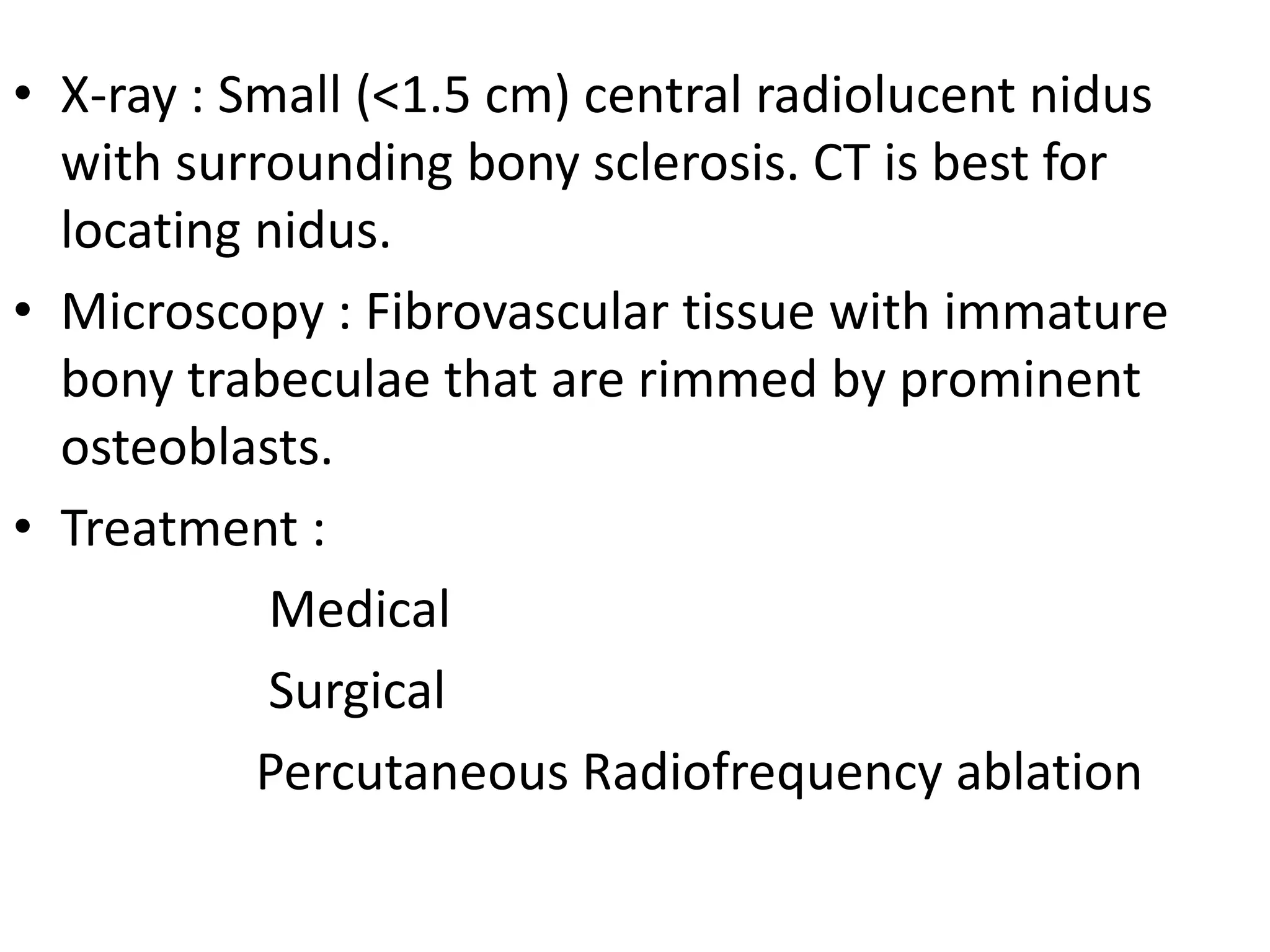
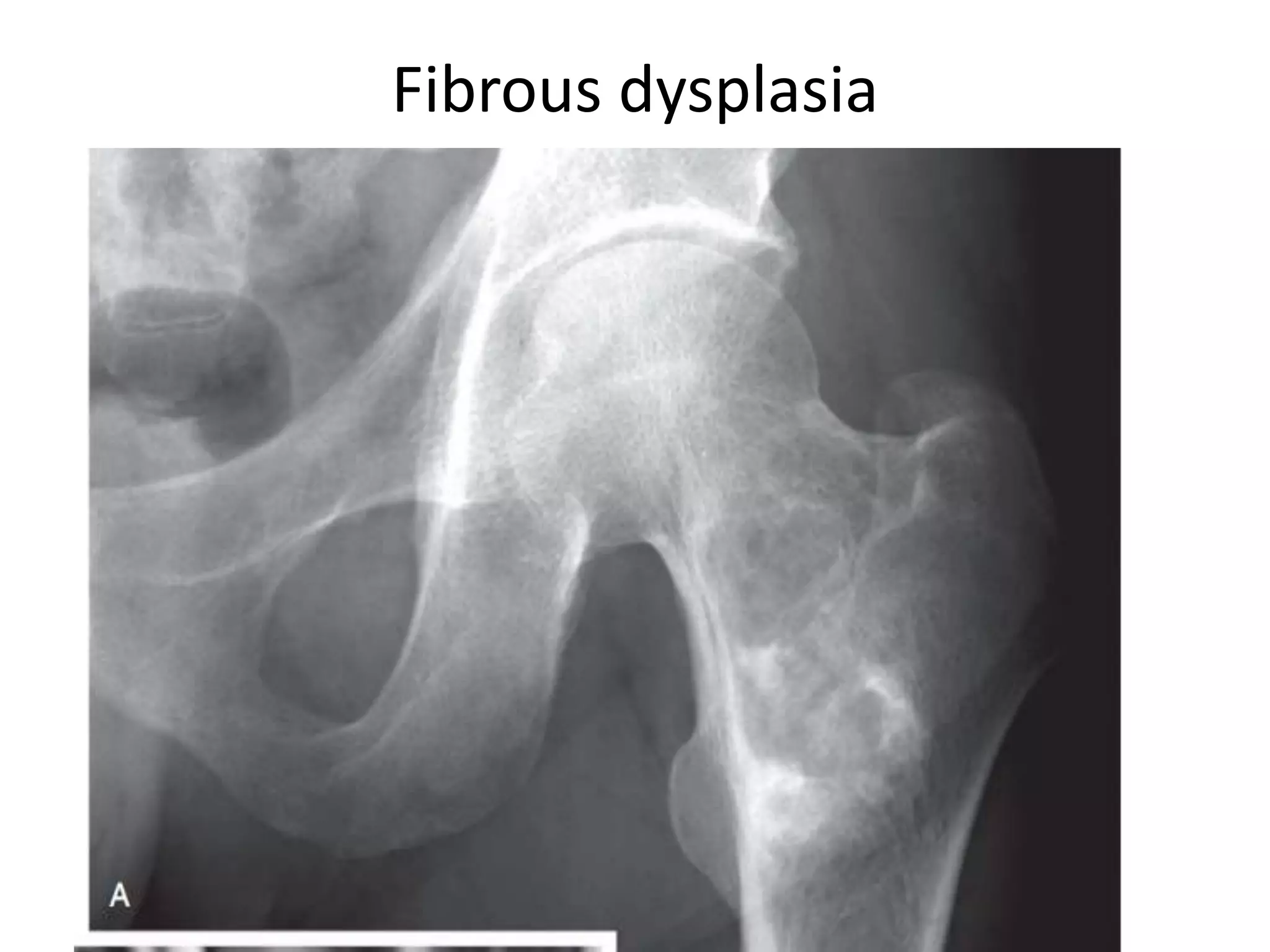
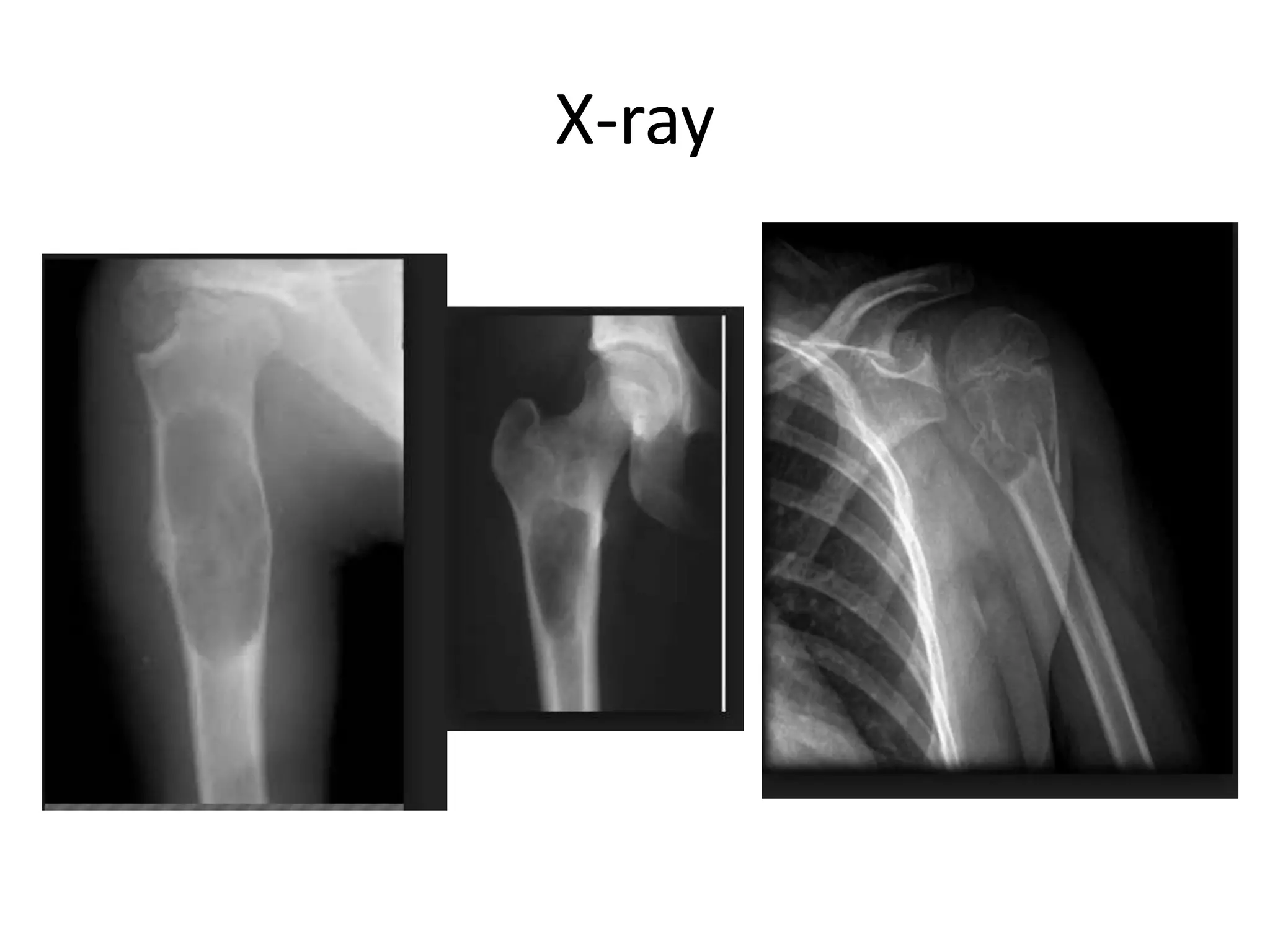
This document provides an overview of common benign bone lesions. It begins with an introduction to bone tumors and their classification as benign or malignant. Several common benign bone tumors are then described in detail, including their clinical features, radiological appearance, diagnosis, treatment, and prognosis. Examples discussed include osteoid osteoma, osteoblastoma, bone islands, chondromas, osteochondromas, chondromyxoid fibroma, chondroblastoma, non-ossifying fibroma, fibrous dysplasia, unicameral bone cyst, aneurysmal bone cyst, and hemangioma. For each lesion, the key presenting symptoms, diagnostic imaging findings, treatment approaches such as surgery or observation, and recurrence risks