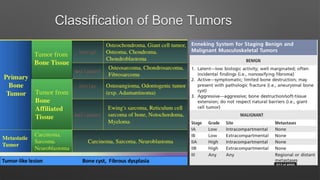
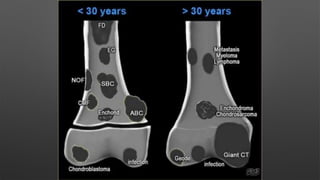
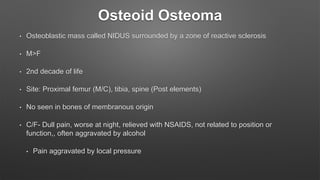
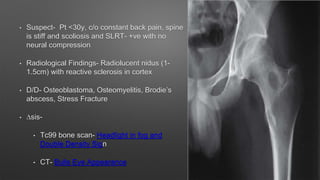
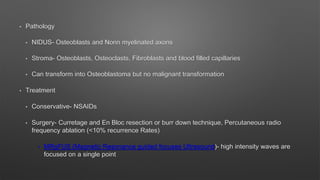
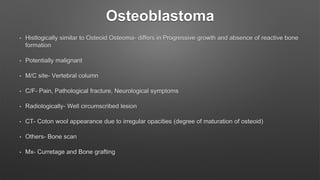
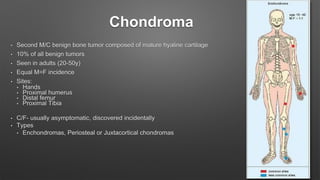
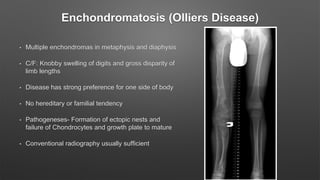
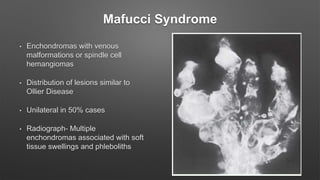
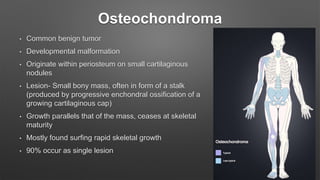
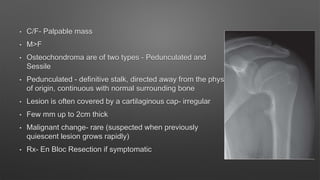
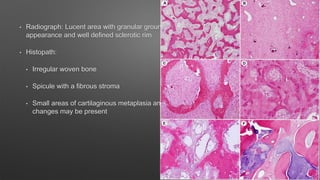
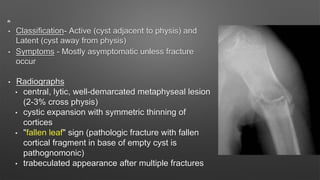
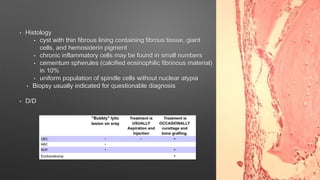
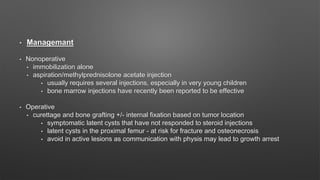
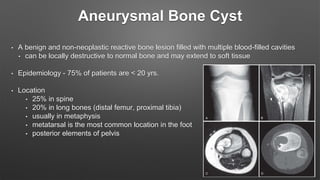
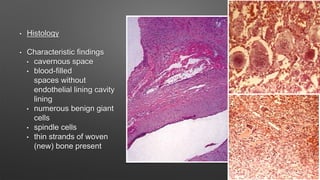
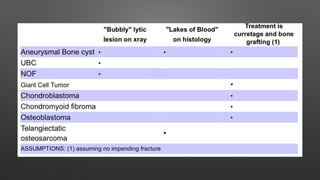
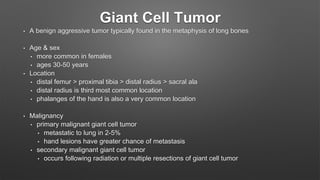
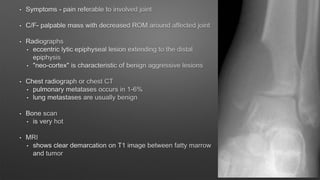
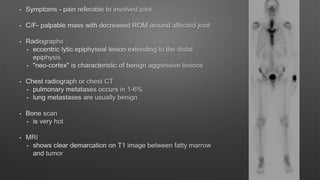
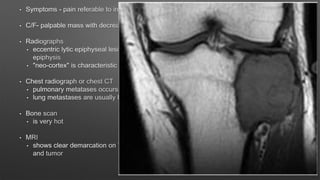
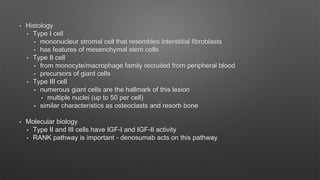
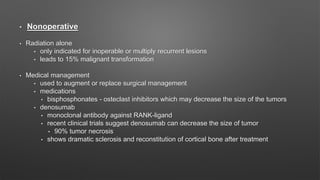
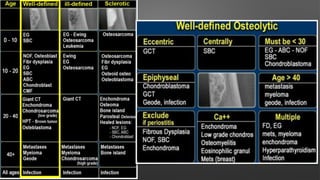
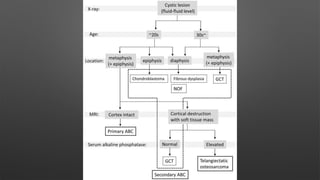
This document summarizes several types of benign bone tumors including osteoid osteoma, osteoblastoma, chondroma, osteochondroma, fibrous dysplasia, and cystic lesions like unicameral bone cyst and aneurysmal bone cyst. It describes the classification, clinical features, radiographic findings, pathology, diagnosis and treatment of these tumors. Malignant tumors like giant cell tumor are also briefly discussed.