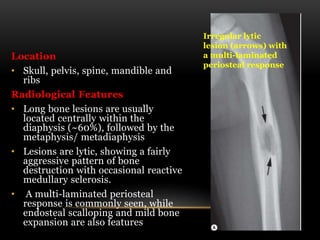
This document discusses various benign bone tumors and provides guidance on their diagnosis and evaluation. It covers several types of bone-forming, cartilage-forming, fibrous, and cystic/vascular lesions. Key information to obtain from patients includes age of presentation, location and characteristics of the lesion seen on imaging studies. Features like well-defined margins, absence of cortical destruction or soft tissue extension suggest benignity. Different tumor types have characteristic appearances on plain radiographs and other imaging modalities that can aid in diagnosis.