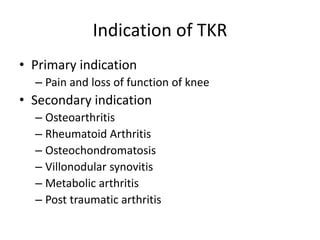
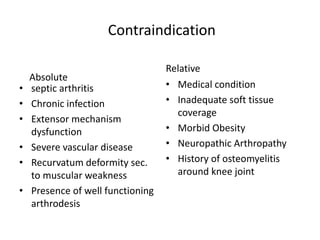
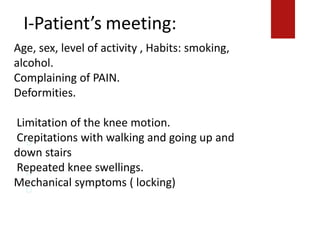
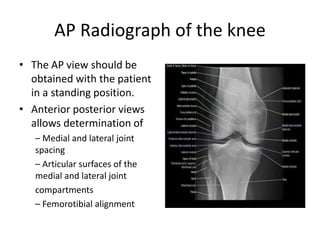
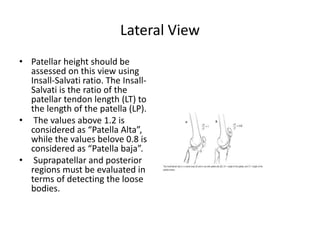
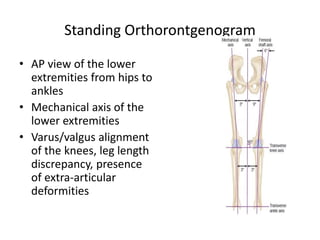
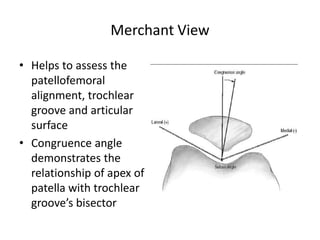
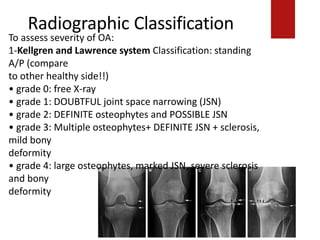
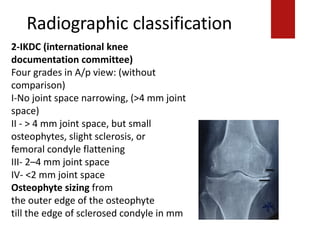
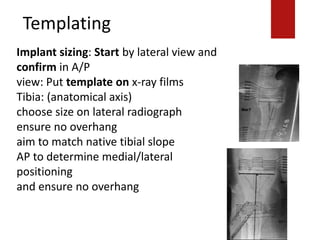
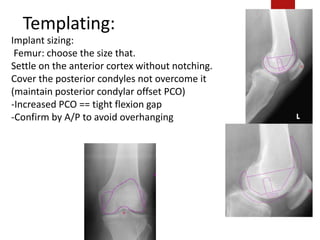
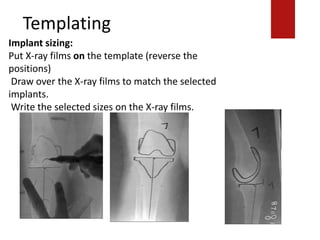
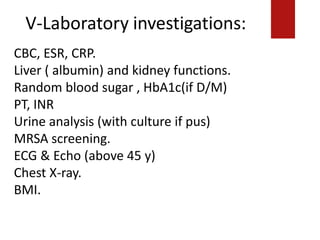
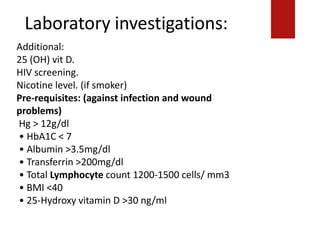
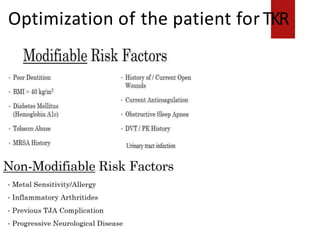
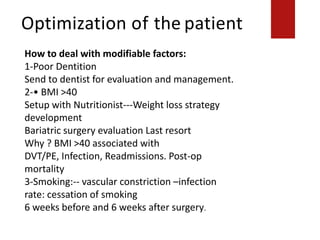
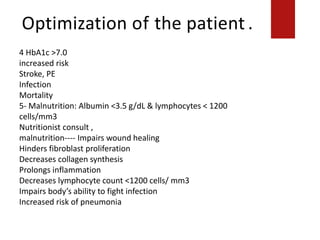
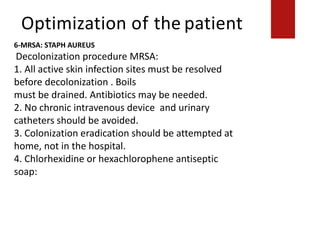
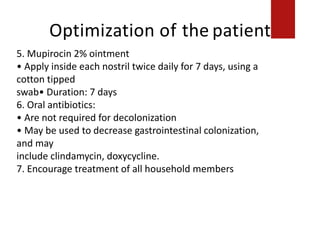
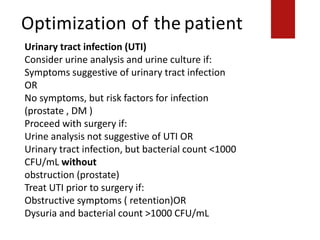
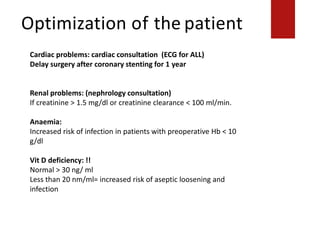
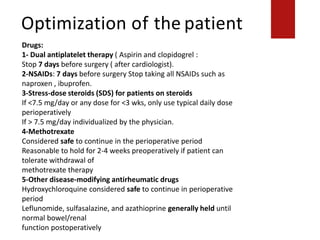
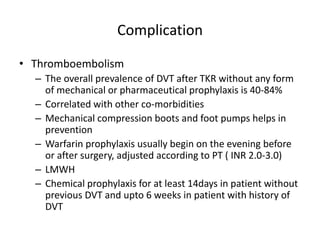
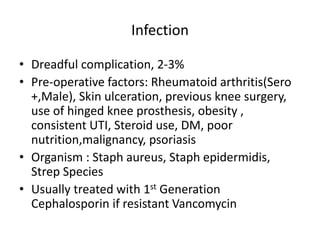
This document discusses the pre-operative evaluation and planning for total knee replacement (TKR) surgery. It covers indications and contraindications for the surgery, patient evaluation including history, physical exam, and imaging, optimization of co-morbidities, surgical planning including templating and sizing, education of the patient, and potential complications of the surgery such as thromboembolism. The goal of the pre-operative process is to adequately prepare the patient and surgical team so that the TKR journey begins with the initial patient meeting and ends safely at the operating room door.